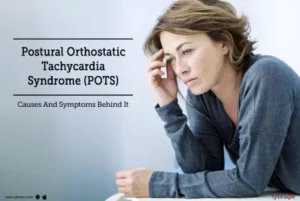
Postural tachycardia syndrome (Pots)
Postural tachycardia syndrome (Pots) is an abnormal increase in heart rate that occurs after sitting up or standing. Some typical symptoms include dizziness and fainting.
It’s sometimes known as postural orthostatic tachycardia syndrome.
Pots affects a range of people but is most common in girls and women aged 15 to 50.
Some people have mild symptoms, while others find the condition affects their quality of life. Pots often improves gradually over time, and there are some medicines and self-care measures that can help.
What happens in Pots
Normally when you sit up or stand, gravity pulls some of your blood down to your belly area, hands and feet.
In response, your blood vessels quickly narrow and your heart rate increases slightly to maintain blood flow to the heart and brain, and prevent blood pressure dropping.
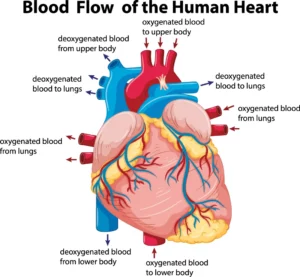
This is all done without needing to think about it, by the autonomic nervous system – the nervous system in charge of automatic body functions.
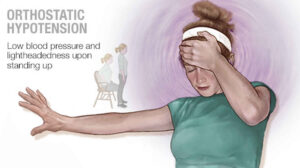
In Pots, the autonomic nervous system does not work properly. There’s a drop in blood supply to the heart and brain when you become upright and the heart races to compensate for this.
Symptoms of Pots
You can develop Pots suddenly, or it can begin gradually.
You can sometimes get symptoms almost immediately, or a few minutes after sitting up or standing. Lying down may relieve some of the symptoms.
Typical symptoms of Pots include:
- dizziness or light-headedness
- fainting
- problems with thinking, memory and concentration – this combination of symptoms is often called “brain fog”
- heart palpitations
- shaking and sweating
- weakness and fatigue (tiredness)
- headaches
- poor sleep
- chest pain
- feeling sick
- shortness of breath
Some people notice that feeling hot, eating, strenuous exercise or having a period can make their symptoms worse.
When to get medical advice
See a GP if you think you have Pots.
The symptoms can have a number of causes, such as medicine or low blood pressure, so it’s a good idea to get a proper diagnosis. Sometimes it can be misdiagnosed as anxiety or panic attacks.

Some doctors may not be aware of Pots, so it may help to print out this page and take it with you to your appointment. A GP will probably need to refer you to a specialist for tests (see below).
Pots UK (a charity for people affected by Pots) has a list of doctors with an interest in Pots that you can use to find a specialist near you. You cannot usually self-refer to these doctors, but you could discuss a referral with a GP.
Tests for Pots
Pots is diagnosed if your heart rate increases by 30 beats a minute (bpm) or more (40bpm in those aged 12 to 19) usually within 10 minutes of standing. This increase continues for more than 30 seconds and is accompanied by other symptoms of Pots.
You may have a range of tests to confirm a diagnosis and rule out other conditions, including:
tilt table test – your heart rate and blood pressure are measured while you lie on a specially designed bed that can be titled upright. The measurements are taken several more times while the bed is slowly tilted into a more upright position
active stand test – your heart rate and blood pressure are measured after lying down, immediately upon standing, then after 2, 5 and 10 minutes
an electrocardiogram (ECG) – a test of your heart’s electrical activity
an echocardiogram – an ultrasound scan of your heart
24-hour ambulatory blood pressure and heart rate monitoring – small devices attached to your belt take regular readings while you’re doing normal activities
blood tests – to test your kidney, liver and thyroid function, and measure blood count and your calcium and glucose levels
Treatments for Pots
Self-care measures can sometimes help to reduce the symptoms of Pots. If these do not work, you may need to take medicine.
Treating an episode
If you suddenly feel faint or dizzy, you can try countering the fall in blood flow by:
lying down and, if you can, raising your legs
crossing your legs in front of each other while standing, rocking up and down on your toes, clenching your buttocks and tummy muscles and/or clenching your fists if you’re unable to lie down
Reducing your symptoms
You may be able to reduce your symptoms in the long term if you:
drink plenty of fluids until your urine is pale yellow
keep active, but pace yourself and choose your exercise carefully – swimming, rowing, lower limb resistance training, walking, jogging and Pilates can help you keep fit and build muscle (strong calf muscles should help pump blood back to your heart)
elevate the head end of your bed, so you’re not sleeping fully horizontal
try wearing support tights or other forms of compression clothing, to improve blood flow in your legs
- avoid long periods of standing
- rise slowly after lying down – sit for a while before standing
- avoid drinking lots of caffeine or alcohol
include more salt in your diet, however this is not advisable if you have high blood pressure or kidney or heart disease, so ask your specialist first
Find out more from the charity Syncope Trust And Reflex anoxic Seizures (STARS) on diagnosis and management of Pots, and Pots UK about self-management programmed.
Medicine
There’s no single medicine used for treating Pots, but your specialist might suggest trying:
- a beta blocker or ivabradine – which decreases the heart rate
- midodrine – which narrows the blood vessels
- fludrocortisone – which decreases the amount of sodium lost in your pee
- a selective serotonin reuptake inhibitor (SSRIs) – a type of antidepressant that can affect how your nervous system works
Causes of Pots
Sometimes the cause of the problem with the nervous system in people with Pots is unknown.
Teenagers will sometimes develop Pots and find it gradually disappears a few years later. Sometimes it can develop suddenly after a viral illness or traumatic event, or during or after pregnancy.
Some of the other known causes are:
hypermobile Ehlers-Danlos syndrome
other underlying conditions – such as diabetes, amyloidosis, sarcoidosis, lupus, Sjogren’s syndrome or cancer
poisoning – with alcohol or certain metals
inheriting a faulty gene that causes too much of the “fight or flight” hormone noradrenaline to be produced
Pots also happens quite commonly alongside chronic fatigue syndrome.
How do I cope emotionally with POTS?
- Be open and honest with loved ones and support groups about your diagnosis of POTS. Talk about your fears, hopes, struggles and challenges with the condition. Encourage the people who support you to learn more about POTS.
- Get enough sleep and eat well to help manage stress.
- Shared medical appointments and POTS support groups (either online or in person) will help reduce the feeling of being alone and different.
- Be careful with social media. Be mindful of the accuracy of any particular website’s data. Some POTS patients find comfort in social media. For others, social media can cause unnecessary and excessive stress and worry.
- Be very cautious of quick solutions from non-medical sources and people. Quick solutions usually don’t help POTS and can even cause more emotional distress.
- We recommend counselling to help you learn to cope with a chronic health condition. Counselling may help to control other co-existing mental health issues that may negatively influence POTS.
- Meditate or take even just a few minutes of a time-out to help reduce some of your POTS symptoms.
- Emotions can have a significant influence on your daily life and health. Identifying them can be useful if you are talking with a counsellor or POTS support group.
Reference
https://my.clevelandclinic.org/health/diseases/16560-postural-orthostatic-tachycardia-syndrome-pots