Hypomania is a condition in which you display a revved-up energy or activity level, mood, or behavior. The new “energized you” is recognized by others as beyond your usual self. Hypomania is a less severe form of mania, and both are commonly part of bipolar disorder. Treatments include psychotherapy, medication, and self-care strategies.
OVERVIEW
What is hypomania?
Hypomania is a condition in which you have a period of abnormally elevated, extreme changes in your mood or emotions, energy level, or activity level. This energized level of energy, mood, and behavior must be a change from your usual self and be noticeable by others.
Hypomania is a symptom of bipolar disorder, but can also be a symptom of other mental health conditions.
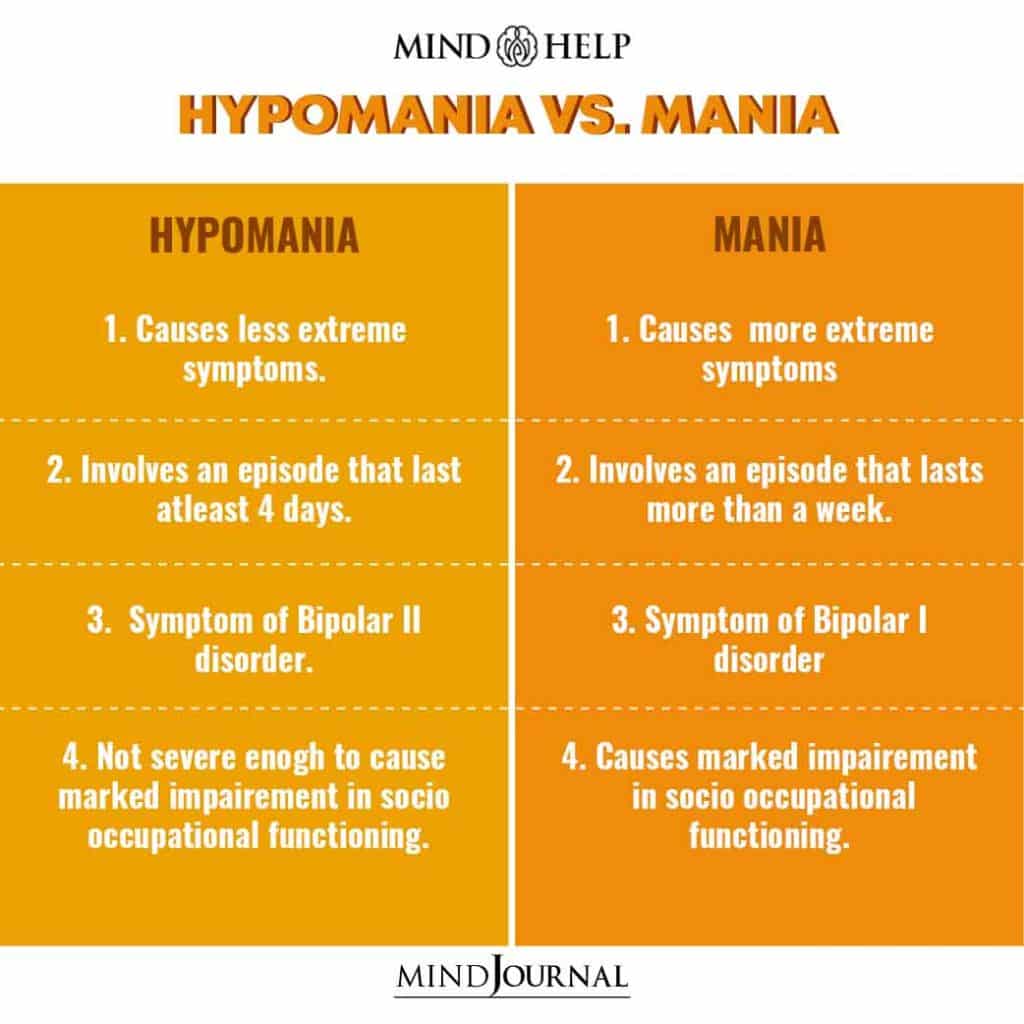
What’s the difference between hypomania and mania?
Hypomania is a less severe form of mania. The criteria that healthcare professionals use to make the diagnosis of either hypomania or mania is what sets them apart. For complete knowledge read the differences given below by Pritish Kumar:
What triggers a hypomanic episode?
- Each person’s triggers may be different. Some common triggers include:
- A highly stimulating situation or environment (e.g., lots of noise, bright lights, large crowds).
- A major life change (e.g., divorce, marriage, job loss).
- Lack of sleep.
- Substance use, such as recreational drugs or alcohol.
It’s smart to develop a list of your triggers to know when a hypomanic episode may be starting. Since hypomania doesn’t cause severe changes in your activity level, mood or behavior, it may be helpful to ask family and close friends whom you trust and have close contact with to help identify your triggers. They may notice changes from your usual self more easily than you do. Share your trigger list with your close, trusted friends so they can tell when you might need help.
How long does a hypomanic episode last?
According to the criteria for hypomania, hypomania must last at least four days. But it can last up to several months.
What happens after a hypomanic episode?
After a hypomanic episode you may:
- Feel happy or embarrassed about your behavior.
- Feel overwhelmed by all the activities you’ve agreed to take on.
- Have only a few or unclear memories of what happened during your manic episode.
- Feel very tired and need sleep.
- Feel depressed (if your hypomania is part of bipolar disorder).
SYMPTOMS AND CAUSES
What are the symptoms of hypomania?
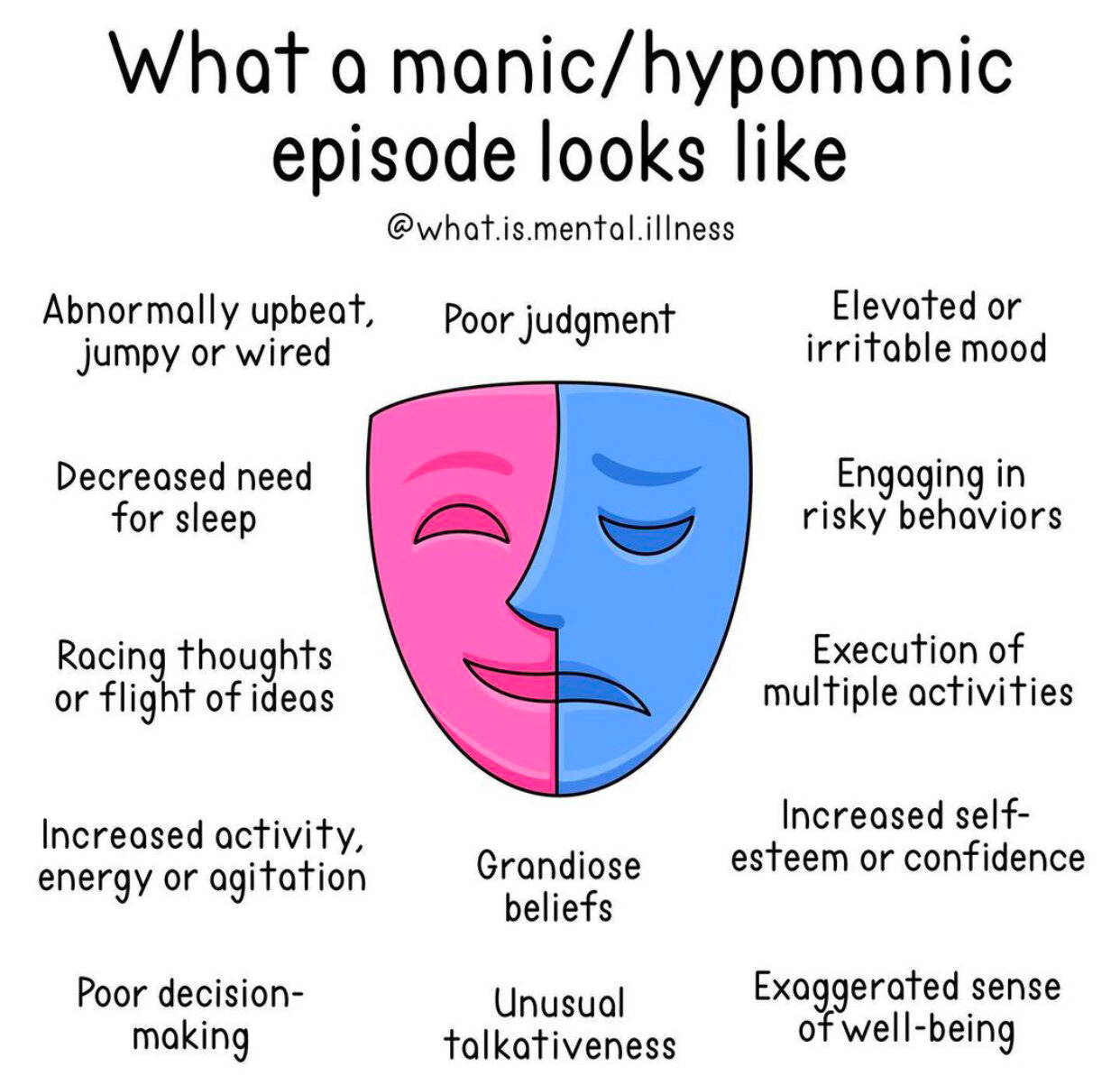
Symptoms of a hypomanic episode are the same but less intense than mania. Hypomanic symptoms, which vary from person to person, include:
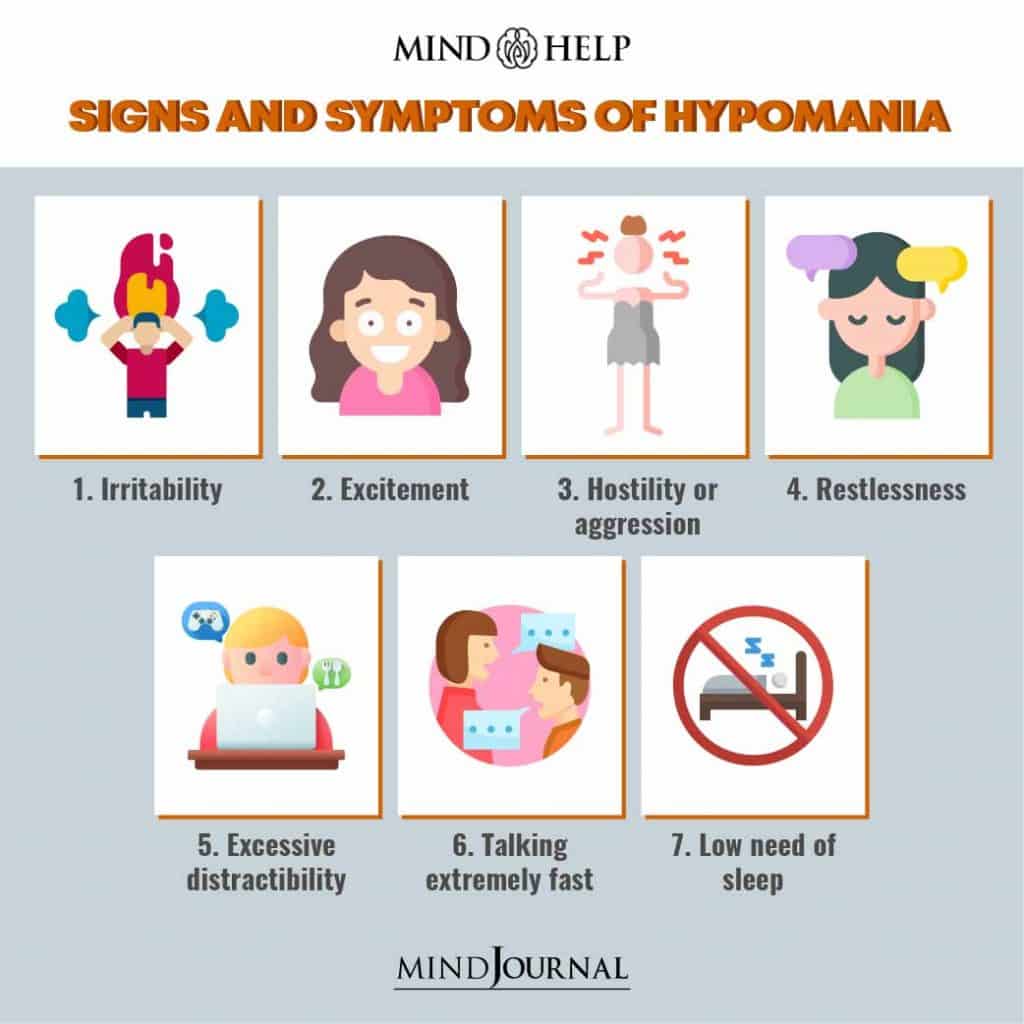
- Having an abnormally high level of activity or energy.
- Feeling extremely happy, and excited.
- Not sleeping or only getting a few hours of sleep but still feeling rested.
- Having inflated self-esteem, thinking you’re invincible.
- Being more talkative than usual. Talking so much and so fast that others can’t interrupt.
- Having racing thoughts — having lots of thoughts on lots of topics at the same time (called a “flight of ideas”).
- Being easily distracted by unimportant or unrelated things.
- Being obsessed with and completely absorbed in an activity you’re focusing on.
- Displaying purposeless movements, such as pacing around your home or office or fidgeting when you’re sitting.
- Showing impulsive behavior that can lead to poor choices, such as buying sprees, reckless sex, or foolish business investments.
Bipolar Hypomania
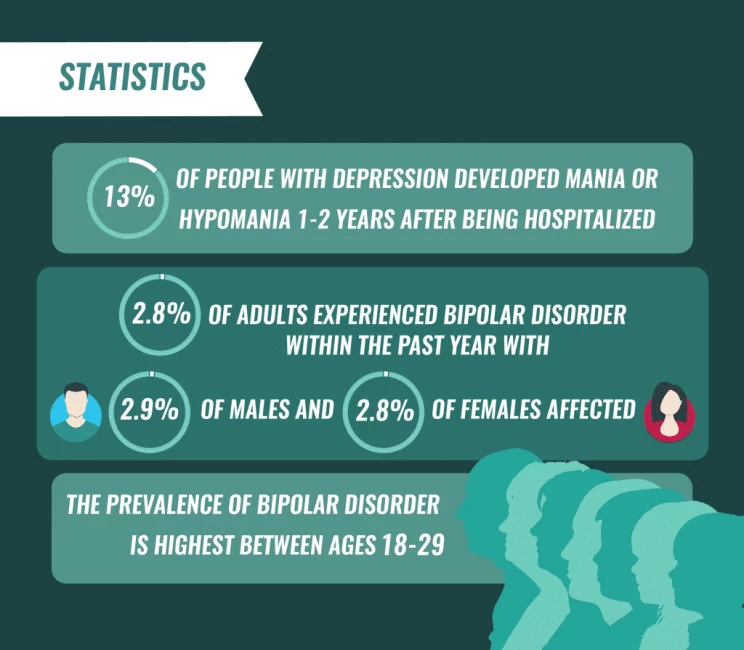
To be diagnosed with bipolar I or bipolar II disorder, a person must generally experience both depressive and manic and/or hypomanic episodes.6 Experiencing symptoms associated with hypomania and depression without mania suggests bipolar II disorder. Other factors may determine if another diagnosis is more appropriate, such as cyclothymia.
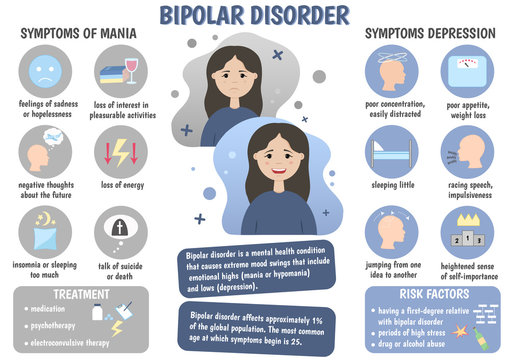
Bipolar hypomania is considered present when a person experiences at least three of the following symptoms accompanied by a persistently elevated mood or four of these symptoms in association with a sustained irritable mood:
- Easily distracted
- Excessive involvement in activities with a high potential for negative consequences (such as spending sprees, gambling, sexual indiscretions, or risky financial investments)
- Feeling driven to accomplish specific goals
- Fidgetiness, pacing, or restlessness (also known as psychomotor agitation)
- Flight of ideas or feeling like your thoughts are racing
- Grandiose thinking, meaning unrealistic thoughts about your powers, talents, or abilities
- Reduced need for sleep without feeling tired
- Unusual talkativeness or feeling pressured to keep talking
Hypomania and bipolar disorder are diagnosed separately, so receiving a diagnosis of hypomania does not necessarily mean also being diagnosed with bipolar disorder and vice versa.
Causes of Hypomania
What’s the difference between feeling good vs hypomania?
It takes time to know the difference. Everyone enjoys being happy and feeling good. But feeling good doesn’t always mean you are good. Over time, you’ll start to understand yourself and learn the warning signs that you may be starting to have an elevated mood that is different from just feeling good.
Ask family and close friends whom you trust, and have frequent contact with, to give you feedback. Ask them to tell you when they see beyond normal changes in your mood or behaviors.
What does hypomania feel and look like?
What hypomania feels like and looks like will be different for each person. Some examples of things you might feel and/or do include:
- Get into an intense cleaning frenzy and clean all surfaces of every room in your house.
- Stay up until 3 a.m. or don’t go to bed at all and not feel tired the next morning.
- Start a project, or more than one project, and work non-stop on these projects for 20 hours straight.
- Feel that you can’t fail at anything you want to do, even if you have no training or experience.
- Call and text all your friends all day and night and post a large number of pictures and comments on social media.
- Quickly jump from subject to subject when talking, and talking very fast.
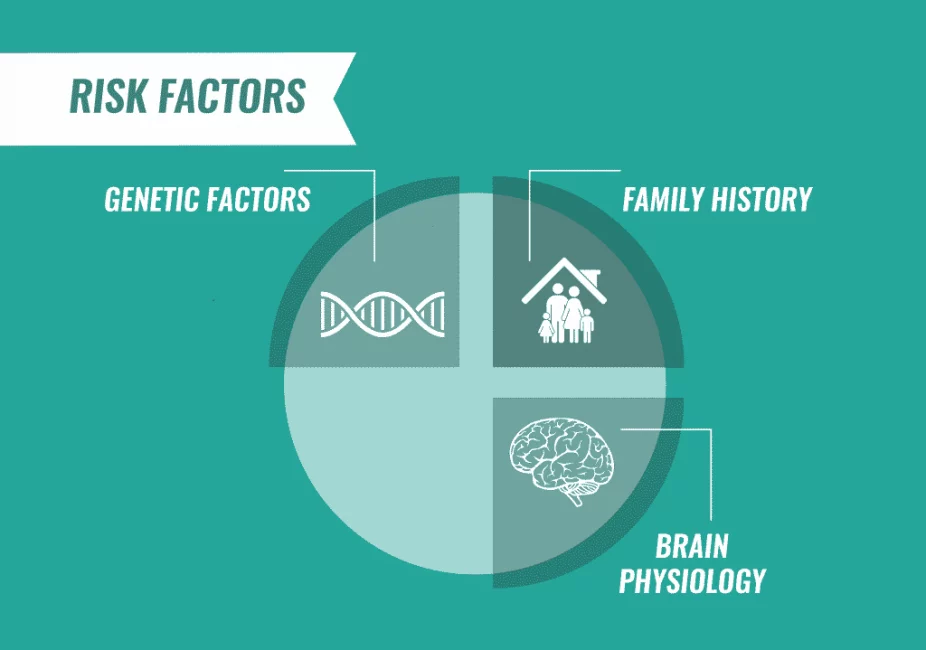
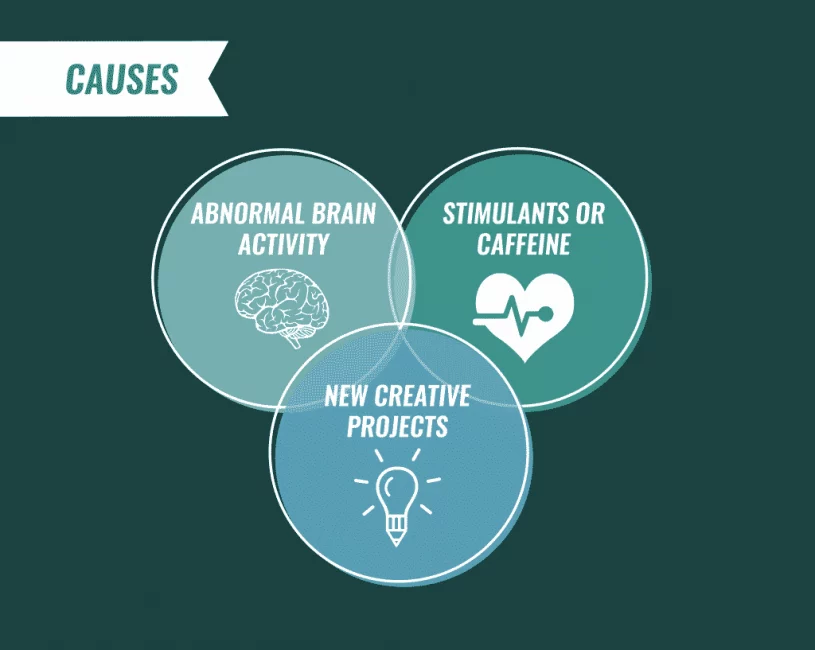
What causes hypomania?
Scientists aren’t completely sure what causes hypomania. However, several factors are thought to contribute. Causes differ from person to person.
Causes may include:
Family history. If you have a family member with bipolar illness, you have an increased chance of developing mania. This is not definite though. You may never develop mania even if other family members have.
- Chemical imbalance in your brain.
- A side effect of a medication (such as some antidepressants), alcohol, or recreational drugs.
- A significant change in your life, such as a divorce, house move, or death of a loved one.
- Difficult life situations, such as trauma or abuse, or problems with housing, money, or loneliness.
- High stress level and inability to manage it.
- Lack of sleep or changes in sleep pattern.
As a symptom of mental health problems including cyclothymia, seasonal affective disorder, postpartum psychosis, schizoaffective disorder, or other physical or neurologic condition such as brain injury, brain tumors, stroke, dementia, lupus, or encephalitis.
Coping With Hypomania
If you’ve been experiencing hypomania-like symptoms, make an appointment with a mental healthcare provider such as a psychiatrist. A mental health professional with experience in diagnosing mood disorders can determine if a diagnosis of hypomania is accurate and whether it’s a symptom of underlying bipolar disorder.
:max_bytes(150000):strip_icc()/hypomania-vs-mania-5196831-Final-d1d880b3916b4dca8b5e6caa3f13817b.jpg)
In the meantime, here are a few tips to help you cope with symptoms of hypomania:
- Educate yourself. The more you learn about hypomania and your symptoms and triggers, the easier it becomes to manage your condition.
- Keep a mood diary. Writing in a journal or using an app can help you chart your moods so you and a healthcare provider can work together to keep your hypomanic episodes under control.
- Stay the treatment course. If you do have bipolar disorder, seeking treatment and complying with your treatment is important to managing hypomania.
- Ask for support. Whether you reach out to trusted friends and family members or join a support group for people with similar symptoms, it can be beneficial to ask for help.
DIAGNOSIS AND TESTS
How is hypomania diagnosed?
Your healthcare provider will ask about your medical history, family medical history, current prescriptions, non-prescription medications, and any herbal products or supplements you take. Your provider may order blood tests and body scans to rule out other conditions that may mimic mania. One such condition is hyperthyroidism. If other diseases and conditions are ruled out, your provider may refer you to a mental health specialist
To be diagnosed with hypomania, your mental health specialist may follow the criteria of the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, DSM-5. Their criteria for the manic episode are:
You have an abnormal, long-lasting elevated expression of emotion along with a high degree of energy and activity that lasts for at least four consecutive days and is present most of the day, nearly every day.
You have three or more symptoms to a degree that they’re a noticeable change from your usual behavior.
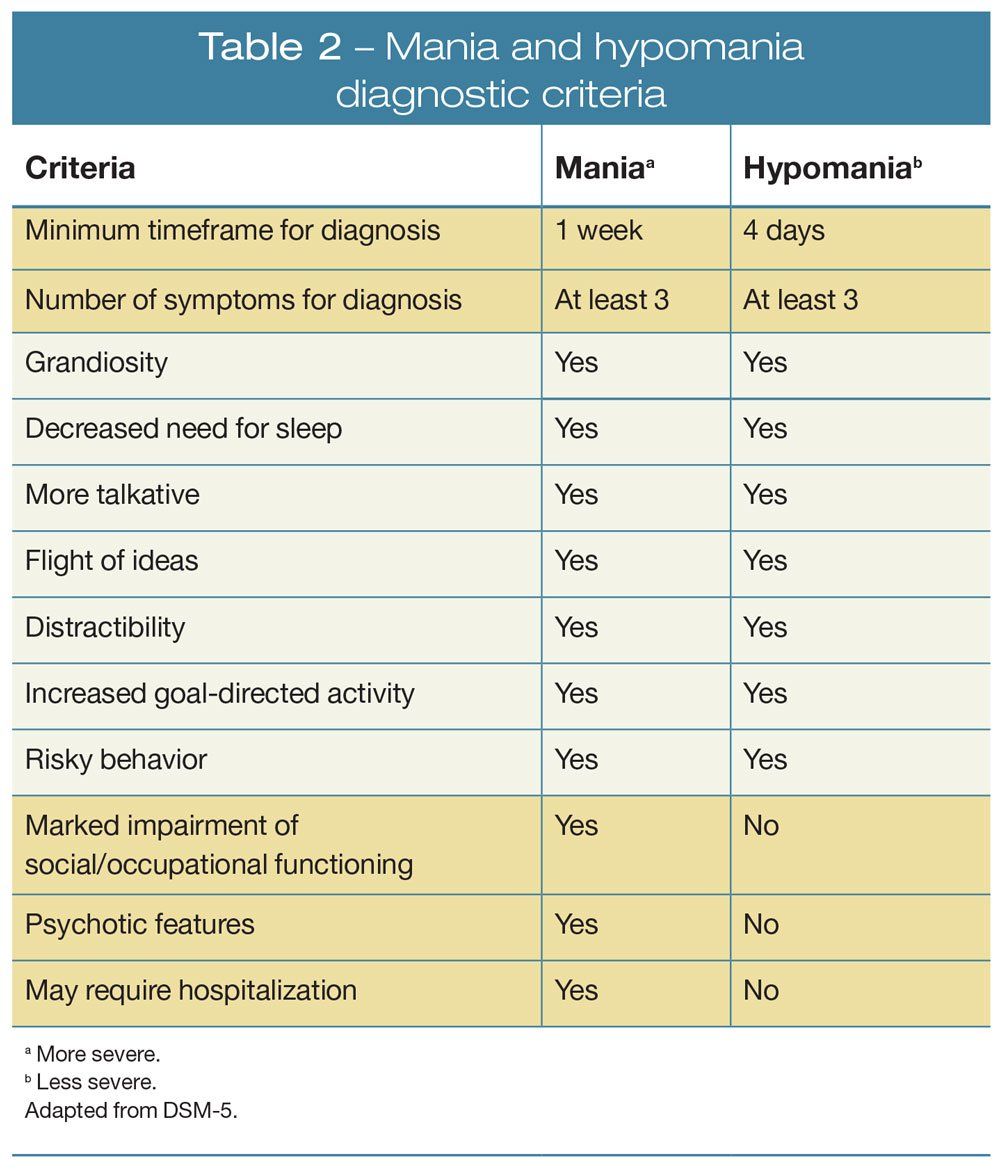
The hypomanic episode is not severe enough to significantly interfere with your social, work, or school functioning and there’s no need for hospitalization.
The hypomanic episode can’t be caused by the effects of a substance (medications or drug abuse) or another medical condition.
If you have hypomania, you don’t have thoughts that are out of step with reality — you don’t have false beliefs (delusions) or false perceptions (hallucinations). If you do have these symptoms of psychosis, your diagnosis is mania.
MANAGEMENT AND TREATMENT
How is hypomania treated?
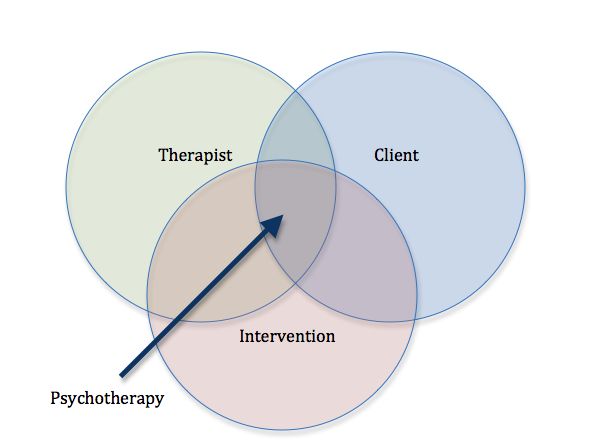
Hypomania is treated with psychotherapy, antipsychotic medications, and mood stabilizers.
/psychotherapy-4157172-FINAL-c8cdb021acb1432d9dffa76a8bfd7f50.png)
Psychotherapy
Psychotherapy involves a variety of techniques. During psychotherapy, you’ll talk with a mental health professional who will help you identify hypomania symptoms and triggers and learn ways to cope with or lessen the effects of hypomanic episodes.

Medications
Antipsychotic medication choices include:
- Aripiprazole (Abilify®).
- Lurasidone (Latuda®).
- Olanzapine (Zyprexa®).
- Quetiapine (Seroquel®).
- Risperridone (Risperdal®).
Mood stabilizers include:
- Lithium.
- Valproate (Depakote®).
- Carbamazepine (Tegretol®).
(If you’re pregnant or plan to become pregnant, let your provider know. Valproate can increase the chance of birth defects and learning disabilities and shouldn’t be prescribed to individuals who can become pregnant.)
- Sometimes antidepressants are also prescribed.
- Managing hypomania without medications
If your hypomania is mild, you may be able to cope without medications. Your healthcare provider may suggest having a greater focus on self-care to stay as healthy as possible.

Suggested actions may include:
- Go to bed at the same time each night and get plenty of sleep (six to nine hours).
- Avoid stimulating triggers such as coffee, tea, colas, sugar, and noisy and crowded environments.
- Eat a healthy diet, such as the Mediterranean or Dash diet.
- Get 30 minutes of exercise on most days of the week. Even two short walks a day are beneficial.
- Don’t use illegal or recreational drugs or alcohol.
- Learn ways to relax. Yoga, meditation, listening to calming music, and aromatherapy are a few examples.
Take all medications as prescribed or instructed on the package labeling. If you think you’re having side effects or new side effects to a medication, call your provider. Never stop taking — or change the dose — of prescription medication without talking to your provider first. Make sure they know all supplements, herbal products, and vitamins you take.
Join a support group. Ask your provider for contact information for local support groups. You might find it helpful to talk with other people who have similar medical experiences and share problems, ideas for coping, and strategies for living and caring for yourself.
PREVENTION
Can hypomania be prevented?
Episodes of hypomania can’t always be prevented. However, you can learn ways to better manage your symptoms and prevent them from getting worse.
Suggestions on your “to-do list” might include:
Keeping a “mood diary” to become more self-aware of events that trigger an oncoming episode of hypomania. These events are unique to you. Sometimes you can’t recognize your triggers. Ask your trusted, close family and friends to help identify when they see changes in your mood, behavior, and energy level that is different from your usual self.
Following other coping strategies. (See the bulleted list under, “Managing hypomania without drugs,” just above in this article.)
OUTLOOK / PROGNOSIS
What outcome can I expect if I’ve been diagnosed with hypomania?
If you’ve been diagnosed with hypomania, you can have a favorable outcome if you learn about your condition, learn to recognize when you’re having a hypomanic episode, and engage in coping strategies to lessen the severity or prevent events. Always take any prescribed medications as directed by your healthcare provider.
A note from Cleveland Clinic
Being amped up about your life and being in a good mood is usually thought to be a good thing. It can be if that’s how you normally are most of the time. This is what makes hypomania a little tricky to diagnose. The key to a diagnosis of hypomania is that your elevated mood, behavior, or activity level must last at least four days (all day or most of the day) and must rise to a level that’s beyond normal and is noticeable to others. Know that a team of healthcare professionals — your primary care provider, psychologists, and/or psychiatrist — is ready to help you figure this out.
Reference
https://www.verywellmind.com/what-is-hypomania-how-is-it-diagnosed-380313