Pancreas Transplant
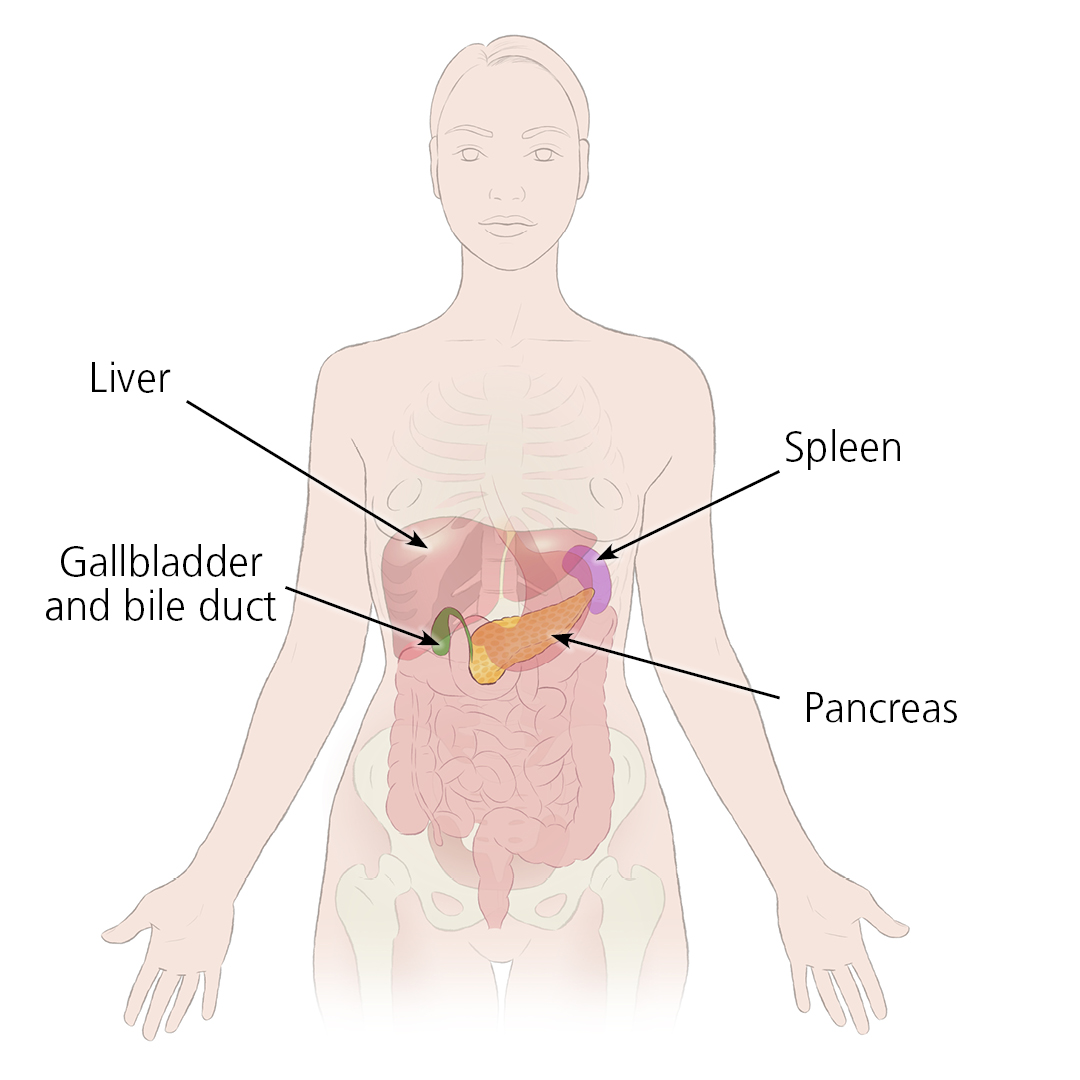
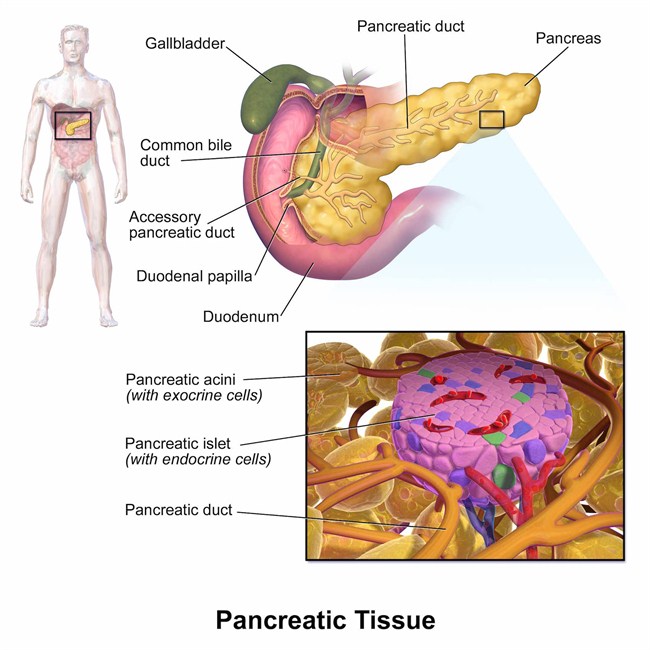
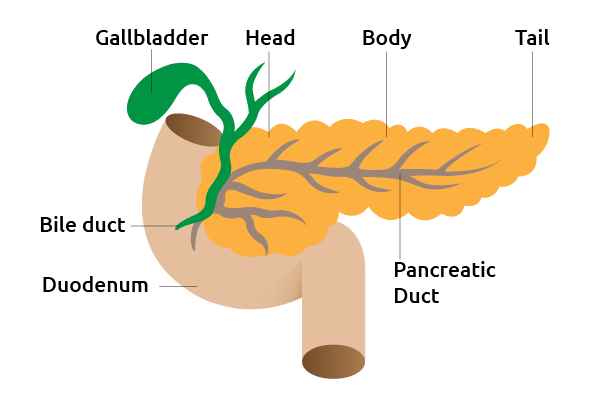
The pancreas is an organ about the size of a hand located in the abdomen in the vicinity of the stomach, intestines, and other organs. It lies behind the stomach and in front of the spine. The pancreas produces juices that help digest food and hormones such as insulin and glucagon that maintain optimal blood sugar levels and help the body to use and store energy from food.
It involves implanting a healthy pancreas (one that produces insulin) into a person whose pancreas no longer can supply sufficient insulin to the body. The healthy pancreas comes from either a deceased donor, or in the form of a partial pancreas from a living donor.
The transplant offers a potential cure for type 1 or insulin-dependent diabetes. A successful pancreas transplant will eliminate the need for insulin injections, reduce or eliminate dietary and activity restrictions due to diabetes, and decrease or eliminate the risk of severe low blood sugar reactions. A pancreas transplant can also help manage the damage to other organs including the kidneys that may result from type 1 diabetes.
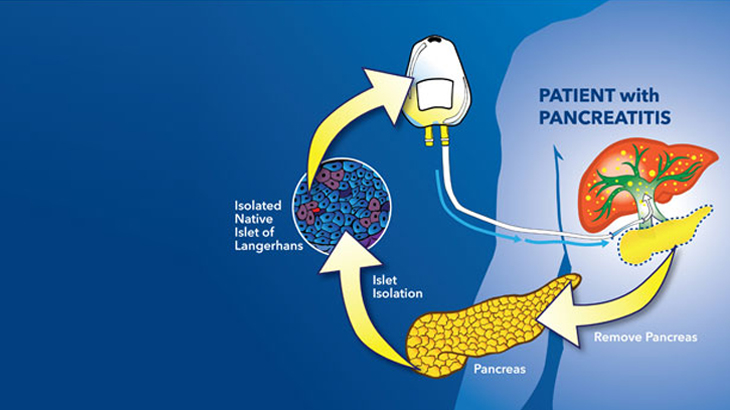
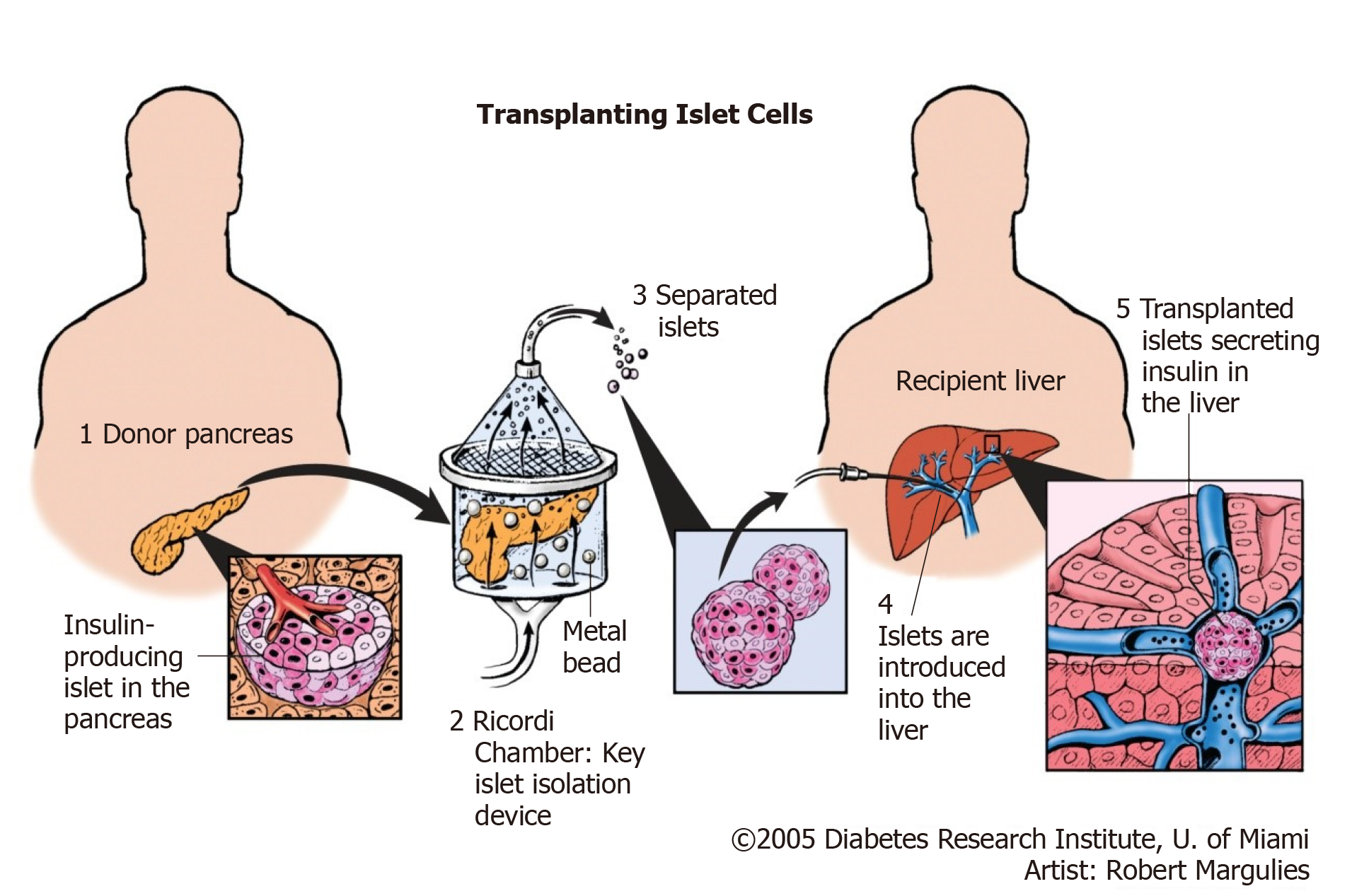
Primarily offered to persons with type 1 with severe kidney disease or other life-threatening consequences from uncontrolled glucose levels. Type 1 diabetes is caused by a loss or malfunction of the insulin producing cells, called pancreatic beta cells. Beta cells (β cells) are a type of cell found in the pancreatic islets of the pancreas. They make up 65-80% of the cells in the islets.
Who Gets Pancreas Transplants
Patients with type 2 diabetes are generally not offered pancreas transplants because their disease results from the body’s inability to use insulin properly, not from an inability to produce in insulin in the pancreas. While the beta cells in type 2 patients may become exhausted and fail, the same fate might await beta cells in transplanted pancreas due to the same factors that caused insulin resistance in the first place.
In this article, Pritish Kumar explains Pancreas transplant with risks & treatments in effective manner.
Type 1 Diabetes
Insufficient insulin As noted above, Type 1 diabetes is caused by a loss or malfunction of the insulin producing cells, called pancreatic beta cells. Damage to beta cells results in an absence or insufficient production of insulin produced by the body. Most cases of type 1 diabetes have an autoimmune basis where the immune system mistakenly attacks and destroys beta cells.
People with type 1 diabetes have very little or no insulin and need to take insulin everyday. Insulin therapy is life-saving. However, most people with type 1 diabetes continue to have blood glucose levels above normal. This puts them at risk for the long-term complications of diabetes such as diabetic retinopathy, an eye disease that can cause poor vision and blindness, and diabetic nephropathy, a kidney disease that can lead to kidney failure.
Some people have what doctors call labile, or brittle, diabetes. Blood glucose levels swing from high to low despite the best insulin plans. Those who are able to keep their blood glucose levels near normal often have trouble with low blood glucose (hypoglycemia).

Over time, some lose awareness of the early symptoms that warn them that their blood glucose level is dropping. This is called hypoglycemia unawareness and raises the risk of severe hypoglycemia. Hypoglycemia unawareness is a life-threatening condition that is not easily treatable with medication and is characterized by reduced or absent warning signals for hypoglycemia. Some Type 1 diabetic patients have been known to set their alarms to wake them several times a night out of fear they may have a catastrophic hypoglycemic episode while asleep.
Considerations in Patients Considering Pancreas Transplants
Although a pancreas transplant offers a potential cure for type 1 diabetes, the side effects of anti-rejection medications required after transplant can be more serious than type 1 diabetes itself. Therefore the risks of the transplant must be outweighed by benefits of getting the transplant. When one of more the following apply, a pancreas transplant may be considered a viable treatment option.
Type 1 diabetes not controlled with standard treatment
- Frequent severe insulin reactions
- Very poor blood sugar control
- Hypoglocemia Unawareness
- Severe kidney damage
Types of Pancreas Transplants
There are three main types of pancreas transplantation:
Pancreas transplant alone, for the patient with type 1 diabetes who usually has severe, frequent hypoglycemia, but adequate kidney function.
Simultaneous pancreas-kidney transplant (SPK), when the pancreas and kidney are transplanted simultaneously from the same deceased donor. One of the most serious complications of type 1 diabetes is end-stage renal disease (ESRD) or end-stage kidney disease, which may require a kidney transplant. A kidney transplant without a pancreas transplant means you must take antirejection medication for the kidney and continue to take insulin.The possibility of diabetes damaging the new kidney and other organs also remains. Successful combined kidney-pancreas transplants prevent diabetic damage in newly transplanted kidneys as well as eliminate the need for insulin therapy. In the best case scenario, a patient would receive a new kidney and pancreas from the same donor.
Pancreas-after-kidney transplant (PAK), when a cadaveric, or deceased, donor pancreas transplant is performed after a previous, and different, living or deceased donor kidney transplant.
Risks
Complications of the procedure
Transplant surgery carries a risk of significant complications, including:
- Blood clots
- Bleeding
- Infection
- Excess sugar in the blood or other metabolic problems
- Urinary complications, including leaking or urinary tract infections
- Failure of the donated pancreas
- Rejection of the donated pancreas
- Anti-rejection medication side effects

After the surgery, you take medications for the rest of your life to help prevent your body from rejecting the donor pancreas. These anti-rejection medications can cause a variety of side effects, including:

- Bone thinning
- High cholesterol
- High blood pressure
- Nausea, diarrhea or vomiting
- Sensitivity to sunlight
Other side effects may include:
- Puffiness
- Weight gain
- Swollen gums
- Acne
- Excessive hair growth or loss
Anti-rejection drugs work by suppressing your immune system. These drugs also make it harder for your body to defend itself against infection and disease.
How you prepare
Choosing a transplant center
If your doctor recommends a pancreas transplant, you’ll be referred to a transplant center. You’re also free to select a transplant center on your own or choose a center from your insurance company’s list of preferred providers.

When you consider transplant centers, you may want to:
- Learn about the number and type of transplants the center performs each year
- Ask about the transplant center’s organ donor and recipient survival rates
- Compare transplant center statistics through the database maintained by the Scientific Registry of Transplant Recipients
- Consider other services provided by the transplant center, such as support groups, travel arrangements, local housing for your recovery period and referrals to other resources
After you select a transplant center, you need an evaluation to determine whether you meet the center’s eligibility requirements.
When the transplant team assesses your eligibility, they’ll consider the following:
- Are you healthy enough to have surgery and tolerate lifelong post-transplant medications?
- Do you have any medical conditions that would hinder the success of the transplant?
- Are you willing and able to take medications and follow the recommendations of the transplant team?
If you need a kidney transplant, too, the transplant team will determine whether it’s better for you to have the pancreas and kidney transplants during the same surgery, or to have the kidney transplant first, followed by the pancreas transplant later. The option that’s right for you depends on the severity of your kidney damage, the availability of donors and your preference

Once you are accepted as a candidate for a pancreas transplant, your name will be placed on a national list of people awaiting a transplant. The waiting time depends on your blood group and how long it takes for a suitable donor — one whose blood and tissue types match yours — to become available.
The average wait for a pancreas transplant is about 20 months. The average wait for a simultaneous kidney-pancreas transplant is about 14 months.

Stay healthy
Whether you wait for a donated pancreas to become available or your transplant surgery is already scheduled, it’s important to stay as healthy as possible to increase your chances of a successful transplant.
- Take medications as prescribed.
- Follow diet and exercise guidelines, and maintain a healthy weight.
- If you smoke, make a plan to quit. Talk to your doctor if you need help quitting.
- Keep all appointments with your health care team.
- Stay involved in healthy activities, including those that benefit emotional health, such as relaxing and spending time with family and friends.
If you wait for a donated pancreas, make sure the transplant team knows how to reach you at all times.
Once a donor pancreas is available, it must be transplanted into a recipient within 18 to 24 hours. You should keep a packed hospital bag handy and make arrangements for transportation to the transplant center in advance.
What you can expect
During the procedure
Surgeons perform pancreas transplants with general anesthesia, so you are unconscious during the procedure. The anesthesiologist or anesthetist gives medication as a gas to breathe through a mask or injects a liquid medication into a vein.

After you are unconscious
- An incision is made down the center of abdomen.
- The surgeon places the donor pancreas and a small portion of the donor’s small intestine into lower abdomen.
- The donor intestine is attached to either small intestine or bladder, and the donor pancreas is connected to blood vessels that also supply blood to legs.
- Your own pancreas is typically left in place to aid digestion.
- If you also receive a kidney transplant, the blood vessels of the new kidney will be attached to blood vessels in the lower part of your abdomen.
- The new kidney’s ureter — the tube that links the kidney to the bladder — will be connected to bladder. Unless your own kidneys are cause complications, such as high blood pressure or infection, they’re left in place.
The surgical team monitors heart rate, blood pressure and blood oxygen throughout the procedure.
Transplant surgery usually lasts about 3 to 6 hours, depending on whether you are have a pancreas transplant alone or kidney and pancreas at the same time.
After the procedure
Stay in the intensive care unit for a couple of days
Doctors and nurses monitor your condition to watch for signs of complications. New pancreas should start working immediately. If your old pancreas has been left in place, it continues to perform its other function
If you have a new kidney, it’ll make urine just like your own kidneys did when they were healthy. Often this starts immediately. But in some cases, urine production may take up to a few weeks to return.

Spend about a week in the hospital
Once you’re stable, you’re taken to a transplant recovery area to continue recuperating. Expect soreness or pain around the incision site while you’re healing.
Have frequent checkups as you continue recovering
After you leave the hospital, close monitoring is necessary for 3 to 4 weeks. Your transplant team will develop a checkup schedule that’s right for you. During this time, if you live in another town, you may need to stay close to the transplant center.

Take medications for the rest of your life
You’ll take a number of medications after your pancreas transplant. Drugs called immunosuppressants help keep your immune system from attacking your new pancreas. Additional drugs may help reduce the risk of other complications, such as infection and high blood pressure, after your transplant.

Results
After a successful pancreas transplant, your new pancreas will make the insulin your body needs, so you’ll no longer need insulin therapy to treat type 1 diabetes.
But even with the best possible match between you and the donor, your immune system will try to reject your new pancreas.
To avoid rejection, you’ll need anti-rejection medications to suppress your immune system. You’ll likely take these drugs for the rest of your life. Because medications to suppress your immune system make your body more vulnerable to infection, your doctor may also prescribe antibacterial, antiviral and antifungal medications.
Signs and symptoms that your body might be rejecting your new pancreas include:
- Belly pain
- Fever
- Excessive tenderness at the transplant site
- Increased blood sugar levels
- Vomiting
- Decreased urination
If you experience any of these symptoms, notify your transplant team immediately
It’s not unusual for pancreas transplant recipients to experience an acute rejection episode within the first few months after the procedure. If you do, you’ll need to return to the hospital for treatment with intensive anti-rejection medications.
Pancreas transplant animation
The donor pancreas is attached to the small intestine with a portion of the donor’s small intestine. Once the new donor pancreas is in place, it replaces the function of the diseases pancreas by releasing insulin and other enzymes into the gastrointestinal tract.
Pancreas transplant survival rates
Survival rates vary by procedure type and transplant center. The Scientific Registry of Transplant Recipients maintains current statistics regarding transplantation for all U.S. transplant centers.
Pancreas rejection rates tend to be slightly higher among pancreas-only transplant recipients. It’s unclear why results are better for those who receive a kidney and pancreas at the same time. Some research suggests that it may be because it’s more difficult to monitor and detect rejection of a pancreas alone versus a pancreas and a kidney.
If your new pancreas fails, you can resume insulin treatments and consider a second transplant. This decision will depend on your current health, your ability to withstand surgery and your expectations for maintaining a certain quality of life.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Coping and Support
You may feel anxious or overwhelmed while waiting for a transplant. Or you may have concerns about rejection, returning to work or other issues after a transplant. Seeking the support of friends and family members can help you cope during this time.
Your transplant team can also assist you with other useful resources and coping strategies throughout the transplant process. You might:
- Join a support group for transplant recipients. Talking with others who have shared your experience can ease concerns and anxiety.
- Share your experiences on social media. Engaging with others who have had a similar experience may help you adjust to your changing situation.
- Find rehabilitation services. If you’re returning to work, your social worker may be able to connect you with rehabilitation services provided by your home state’s department of vocational rehabilitation.
- Set realistic goals and expectations. Recognize that life after transplant may not be exactly the same as life before transplant. Having realistic expectations about results and recovery time can help reduce stress.
- Educate yourself. Learn as much as you can about your procedure and ask questions about things you don’t understand. Knowledge is empowering.
New medication options
Researchers actively study medications and treatments for people with pancreas transplants. Current research includes comparing and developing new anti-rejection medication (immunosuppressive) regimens to keep your body from rejecting your new pancreas.
For example, researchers are investigating ways to personalize immunosuppression maintenance regimens by using immune system monitoring.
They also study the possibility of lowering the dose of immunosuppressive medications, such as calcineurin inhibitors, to reduce side effects.
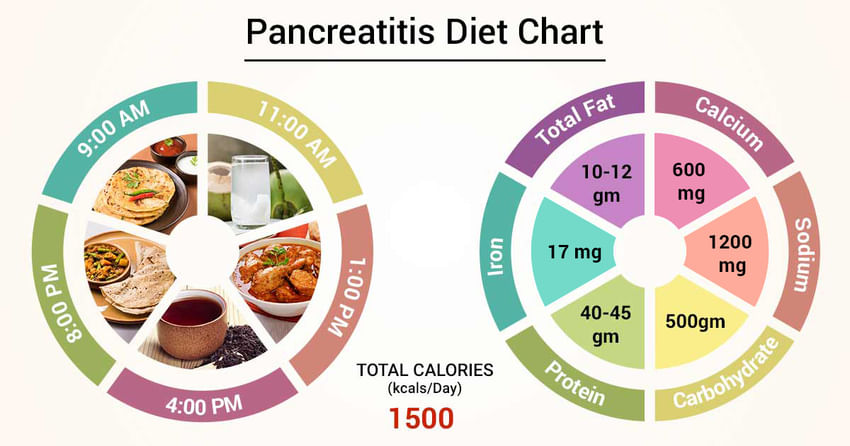
Diet and nutrition
After your pancreas transplant, you may need to adjust your diet to keep your pancreas healthy and functioning well. Maintaining a healthy weight through diet and exercise can help prevent many common post-transplant complications, including infection, heart attacks and bone thinning.

Team typically includes a nutrition specialist (dietitian) who can discuss your nutrition and diet needs and answer any questions you have after your transplant.
Your dietitian can provide you with several healthy food options and ideas to use in your nutrition plan.

Recommendations may include:
- Eat at least five servings of fruits and vegetables each day
- Have lean meats, poultry and fish
- Consume whole-grain breads, cereals and other products
- Having enough fiber in your daily diet
- Drink low-fat milk or eating other low-fat dairy products to help maintain healthy calcium levels

May also recommend:
- Limiting salt and sodium intake by using fresh herbs and spices to season foods and avoiding processed foods
- Restrict unhealthy fats, such as saturated fats in butter and red meats
- Lower your caffeine and avoiding excessive alcohol intake
- Staying hydrated by drinking adequate water and other fluids each day
- Avoiding grapefruit and grapefruit juice, pomegranate and Seville oranges due to their effect on a group of immunosuppressive medications (calcineurin inhibitors)
- Following food safety practices to reduce the risk of infection

Exercise
Physical activity should be a regular part of life after a pancreas transplant. Physical activity can help to continue improving overall physical and mental health.
After a transplant, regular exercise helps boost energy levels and increase strength. It also helps to maintain a healthy weight, reduce stress and prevent common post-transplant complications such as high blood pressure and cholesterol levels.

Transplant team will recommend a physical activity program based on individual needs and goals.
Soon after transplant, walk as much as you can. Then start to incorporate more physical activity into daily life, including participating in at least 30 minutes of moderate exercise five days a week.
Walking, bicycling, swimming, low-impact strength training and other physical activities you enjoy can all be a part of a healthy, active lifestyle after transplant. But be sure to check in with transplant team before starting or changing your post-transplant exercise routine.
Reference
https://transplantsurgery.ucsf.edu/conditions–procedures/pancreas-transplant.aspx
https://www.mayoclinic.org/tests-procedures/pancreas-transplant/about/pac-20384783