Overview
Bipolar disorder (formerly called manic-depressive illness or manic depression) is a mental disorder that causes unusual shifts in mood, energy, activity levels, concentration, and the ability to carry out day-to-day tasks.

There are three types of bipolar disorder. All three types involve clear changes in mood, energy, and activity levels. These moods range from periods of extremely “up,” elated, irritable, or energized behavior (known as manic episodes) to very “down,” sad, indifferent, or hopeless periods (known as depressive episodes).
Sometimes a person might experience symptoms of bipolar disorder that do not match the three categories listed above, which are referred to as “other specified and unspecified bipolar and related disorders.”
If you want to know more about bipolar disorder, read this article with Pritish Kumar.
Bipolar disorder is typically diagnosed during late adolescence (teen years) or early adulthood. Occasionally, bipolar symptoms can appear in children. Bipolar disorder can also first appear during a woman’s pregnancy or following childbirth. Although the symptoms may vary over time, bipolar disorder usually requires lifelong treatment. Following a prescribed treatment plan can help people manage their symptoms and improve their quality of life.
Symptoms
There are several types of bipolar and related disorders. They may include mania or hypomania and depression. Symptoms can cause unpredictable changes in mood and behavior, resulting in significant distress and difficulty in life. Less severe manic periods are known as hypomanic episodes.

- Bipolar I Disorder—defined by manic episodes that last at least 7 days, or by manic symptoms that are so severe that the person needs immediate hospital care. Usually, depressive episodes occur as well, typically lasting at least 2 weeks. Episodes of depression with mixed features (having depressive symptoms and manic symptoms at the same time) are also possible.
- Bipolar II Disorder— defined by a pattern of depressive episodes and hypomanic episodes, but not the full-blown manic episodes that are typical of Bipolar I Disorder.
- Cyclothymic Disorder (also called Cyclothymia)— is defined by periods of hypomanic symptoms as well as periods of depressive symptoms lasting for at least 2 years (1 year in children and adolescents). However, the symptoms do not meet the diagnostic requirements for a hypomanic episode and a depressive episode.
Other types
These include, for example, bipolar and related disorders induced by certain drugs or alcohol or due to a medical condition, such as Cushing’s disease, multiple sclerosis, or stroke.
Bipolar II disorder is not a milder form of bipolar I disorder, but a separate diagnosis. While the manic episodes of bipolar I disorder can be severe and dangerous, individuals with bipolar II disorder can be depressed for longer periods, which can cause significant impairment.
Although bipolar disorder can occur at any age, typically it’s diagnosed in the teenage years or early 20s. Symptoms can vary from person to person, and symptoms may vary over time.

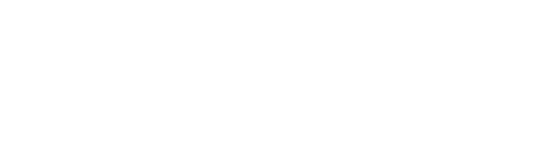
Mania and hypomania
These are two distinct types of episodes, but they have the same symptoms. Mania is more severe than hypomania and causes more noticeable problems at work, school, and social activities, as well as relationship difficulties. Mania may also trigger a break from reality (psychosis) and require hospitalization.
Both a manic and a hypomanic episode include three or more of these symptoms:
- Abnormally upbeat, jumpy or wired
- Increased activity, energy or agitation
- Exaggerated sense of well-being and self-confidence (euphoria)
- Decreased need for sleep
- Unusual talkativeness
- Racing thoughts
- Distractibility
- Poor decision-making — for example, going on buying sprees, taking sexual risks, or making foolish investments
Major depressive episode
Includes symptoms that are severe enough to cause noticeable difficulty in day-to-day activities, such as work, school, social activities, or relationships. An episode includes five or more of these symptoms:
Depressed mood, such as feeling sad, empty, hopeless, or tearful (in children and teens, depressed mood can appear as irritability)
Marked loss of interest or feeling no pleasure in all — or almost all — activities

Significant weight loss when not dieting, weight gain, or decrease or increase in appetite (in children, failure to gain weight, as expected, can be a sign of depression)
- insomnia 0r sleeping too much
- Either restlessness or slowed behavior
- Fatigue or loss of energy
- Feelings of worthlessness or excessive or inappropriate guilt
- Decreased ability to think or concentrate, or indecisiveness
- Thinking about, planning, or attempting suicide
Other features of bipolar disorder
Signs and symptoms of bipolar I and bipolar II disorders may include other features, such as anxious distress, melancholy, psychosis, or others. The timing of symptoms may include diagnostic labels such as mixed or rapid cycling. In addition, bipolar symptoms may occur during pregnancy or change with the seasons.
Symptoms in children and teens
Bipolar disorder can be difficult to identify in children and teens. It’s often hard to tell whether these are normal ups and downs, the results of stress or trauma, or signs of a mental health problem other than bipolar disorder.
/379962-bipolar-disorder-symptoms-and-diagnosis-5b1150af3418c60037552e47.png)
Children and teens may have distinct major depressive or manic or hypomanic episodes, but the pattern can vary from that of adults with bipolar disorder. And moods can rapidly shift during episodes. Some children may have periods without mood symptoms between episodes.
The most prominent signs of bipolar disorder in children and teenagers may include severe mood swings that are different from their usual mood swings.
Diagnosis
Proper diagnosis and treatment can help people with bipolar disorder lead healthy and active lives. Talking with a doctor or other licensed health care provider is the first step. The health care provider can complete a physical exam and order necessary medical tests to rule out other conditions. The health care provider may then conduct a mental health evaluation or provide a referral to a trained mental health care provider, such as a psychiatrist, psychologist, or clinical social worker who has experience in diagnosing and treating bipolar disorder.
/what-is-bipolar-mania-how-is-it-diagnosed-380314_finalcopy-bbe70a3726fe426b9f962c56a24c0036.png)
Mental health care providers usually diagnose the bipolar disorder based on a person’s symptoms, lifetime history, experiences, and, in some cases, family history. Accurate diagnosis in youth is particularly important. You can find tips for talking with your health care provider in the NIMH fact sheet on Taking Control of Your Mental Health: Tips for Talking with Your Health Care Provider.
Bipolar Disorder and Other Conditions
Some bipolar disorder symptoms are similar to those of other illnesses, which can make it challenging for a health care provider to make a diagnosis. In addition, many people may have bipolar disorder along with another mental disorder or condition, such as an anxiety disorder, substance use disorder, or an eating disorder. People with bipolar disorder have an increased chance of having thyroid disease, migraine headaches, heart disease, diabetes, obesity, and other physical illnesses.
Psychosis
Sometimes, a person with severe episodes of mania or depression may experience psychotic symptoms, such as hallucinations or delusions. The psychotic symptoms tend to match the person’s extreme mood. For example:
- People having psychotic symptoms during a manic episode may have the unrealistic belief that they are famous, have a lot of money, or have special powers.
- Certain people having psychotic symptoms during a depressive episode may falsely believe they are financially ruined and penniless, have committed a crime, or have an unrecognized serious illness.
As a result, people with bipolar disorder who also have psychotic symptoms are sometimes incorrectly diagnosed with schizophrenia. When people have symptoms of bipolar disorder and also experience periods of psychosis that are separate from mood episodes, the appropriate diagnosis may be schizoaffective disorder.
Anxiety
It is common for people with bipolar disorder to also have an anxiety disorder.
Attention-Deficit Hyperactivity Disorder (ADHD): It is common for people with bipolar disorder to also have ADHD.
Misuse of Drugs or Alcohol: People with bipolar disorder may misuse alcohol or drugs and engage in other high-risk behaviors at times of impaired judgment during manic episodes. Although the negative effects of alcohol use or drug use may be most evident to family, friends, and health care providers, it is important to recognize the presence of an associated mental disorder.
Eating Disorders: In some cases, people with bipolar disorder also have an eating disorder, such as binge eating or bulimia.
Risk Factors
Researchers are studying the possible causes of bipolar disorder. Most agree that there is no single cause and it is likely that many factors contribute to a person’s chance of having the illness.
Brain Structure and Functioning: Some studies indicate that the brains of people with bipolar disorder may differ from the brains of people who do not have bipolar disorder or any other mental disorder. Learning more about these differences may help scientists understand bipolar disorder and determine which treatments will work best. At this time, health care providers base the diagnosis and treatment plan on a person’s symptoms and history, rather than brain imaging or other diagnostic tests.
Genetics: Some research suggests that people with certain genes are more likely to develop bipolar disorder. Research also shows that people who have a parent or sibling with bipolar disorder have an increased chance of having the disorder themselves. Many genes are involved, and no one gene can cause the disorder. Learning more about how genes play a role in bipolar disorder may help researchers develop new treatments.
Treatments and Therapies
Treatment can help many people, including those with the most severe forms of bipolar disorder. An effective treatment plan usually includes a combination of medication and psychotherapy, also called “talk therapy.”
Bipolar disorder is a lifelong illness. Episodes of mania and depression typically come back over time. Between episodes, many people with bipolar disorder are free of mood changes, but some people may have lingering symptoms. Long-term, continuous treatment can help people manage these symptoms.
Medications
Certain medications can help manage symptoms of bipolar disorder. Some people may need to try several different medications and work with their healthcare provider before finding medications that work best.
Medications generally used to treat bipolar disorder include mood stabilizers and second-generation (“atypical”) antipsychotics. Treatment plans may also include medications that target sleep or anxiety. Health care providers often prescribe antidepressant medication to treat depressive episodes in bipolar disorder, combining the antidepressant with a mood stabilizer to prevent triggering a manic episode.
People taking medication should:
- Talk with their health care provider to understand the risks and benefits of the medication.
- tell their health care provider about any prescription drugs, over-the-counter medications, or supplements they are already taking.
- Report any concerns about side effects to a health care provider right away. The health care provider may need to change the dose or try a different medication.
- Remember that medication for bipolar disorder must be taken consistently, as prescribed, even when one is feeling well.
Avoid stopping a medication without talking to a health care provider first. Suddenly stopping a medication may lead to a “rebound” or worsening of bipolar disorder symptoms. For basic information about medications, visit NIMH’s Mental Health Medications webpage. For the most up-to-date information on medications, side effects, and warnings, visit the U.S. Food and Drug Administration (FDA) Medication Guides website.
Psychotherapy
Also called “talk therapy,” can be an effective part of the treatment plan for people with bipolar disorder. Psychotherapy is a term for a variety of treatment techniques that aim to help a person identify and change troubling emotions, thoughts, and behaviors. It can provide support, education, and guidance to people with bipolar disorder and their families. Treatment may include therapies such as cognitive-behavioral therapy (CBT) and psychoeducation, which are used to treat a variety of conditions.
Treatment may also include newer therapies designed specifically for the treatment of the bipolar disorder, including interpersonal and social rhythm therapy (IPSRT) and family-focused therapy. Determining whether intensive psychotherapeutic intervention at the earliest stages of bipolar disorder can prevent or limit its full-blown onset is an important area of ongoing research.
Other Treatment Options
Some people may find other treatments helpful in managing their bipolar symptoms, including:
Electroconvulsive Therapy (ECT): The therapy is a brain stimulation procedure that can help people get relief from severe symptoms of bipolar disorder. With modern ECT, a person usually goes through a series of treatment sessions over several weeks. It is delivered under general anesthesia and is safe. It can be effective in treating severe depressive and manic episodes, which occur most often when medication and psychotherapy are not effective or are not safe for a particular patient. This can also be effective when a rapid response is needed, as in the case of suicide risk or catatonia (a state of unresponsiveness).
More research is needed to determine the effects of other treatments, including:
Transcranial magnetic stimulation (TMS): TMS is a newer approach to brain stimulation that uses magnetic waves. It is delivered to an awake patient most days for 1 month. Research shows that TMS is helpful for many people with various subtypes of depression, but its role in the treatment of the bipolar disorder is still under study.
Supplements: Although there are reports that some supplements and herbs may help, not enough research has been conducted to fully understand how these supplements may affect people with bipolar disorder.
A health care provider needs to know about all prescription drugs, over-the-counter medications, and supplements a patient is taking. Certain medications and supplements taken together may cause unwanted or dangerous effects.
Beyond Treatment: Things You Can Do
Regular Exercise
Regular aerobic exercise, such as jogging, brisk walking, swimming, or bicycling, helps with depression and anxiety, promotes better sleep, and is healthy for your heart and brain. There is also some evidence that anaerobic exercises such as weightlifting, yoga, and Pilates can be helpful. Check with your health care provider before you start a new exercise regimen.
Keeping a Life Chart
Even with proper treatment, mood changes can occur. Treatment is more effective when a patient and health care provider work together and talk openly about concerns and choices. Keeping a life chart that records daily mood symptoms, treatments, sleep patterns, and life events can help patients and health care providers track and treat bipolar disorder over time. Patients can easily share data collected via smartphone apps – including self-reports, self-ratings, and activity data – with their health care providers and therapists.
Finding Treatment
- A family health care provider or doctor is a good resource and can be the first stop in searching for help. For tips for talking with your health care provider, see NIMH’s Taking Control of Your Mental Health: Tips for Talking with Your Health Care Provider fact sheet.
- For general information on mental health and to find local treatment services, call the Substance Abuse and Mental Health Services Administration (SAMHSA) Treatment Referral Helpline at 1-800-662-HELP (4357).
- The SAMHSA website has a Behavioral Health Treatment Services Locator that can search for treatment information by address, city, or ZIP code.
- Visit NIMH’s Help for Mental Illnesses webpage for more information and resources.
For Immediate Help
If you are in crisis: Call the toll-free National Suicide Prevention Lifeline at 1-800-273-TALK (8255), available 24 hours a day, 7 days a week. The service is available to everyone. All calls are confidential. Contact social media outlets directly if you are concerned about a friend’s social media updates or dial 911 in an emergency.
- If you are thinking about harming yourself or thinking about suicide:
- Tell someone who can help right away.
- Call your licensed mental health professional if you are already working with one.
- Contact your doctor or health care provider.
- Go to the nearest hospital emergency department or call 911.
If a loved one is considering suicide:
- Do not leave him or her alone.
- Try to get your loved one to seek immediate help from a doctor, health care provider, or the nearest hospital emergency room or call 911.
- Remove access to firearms or other potential tools for suicide, including medications.
Coping with Bipolar Disorder
Living with bipolar disorder can be challenging, but there are ways to help make it easier for yourself, a friend, or a loved one.
- Get treatment and stick with it—recovery takes time and it’s not easy. But treatment is the best way to start feeling better.
- Keep medical and therapy appointments and talk with the provider about treatment options.
- Take all medicines as directed.
- Structure activities: keep a routine for eating and sleeping, and make sure to get enough sleep and exercise.
- Learn to recognize your mood swings and warning signs, such as decreased sleep.
- Ask for help when trying to stick with your treatment.
- Be patient; improvement takes time. Social support helps.
- Avoid misuse of alcohol and drugs.
Remember: Bipolar disorder is a lifelong illness, but long-term, ongoing treatment can help control symptoms and enable you to live a healthy life.
Join a Study
Clinical trials are research studies that look at new ways to prevent, detect, or treat diseases and conditions. The goal of clinical trials is to determine if a new test or treatment works and is safe. Although individuals may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.
Researchers at NIMH and around the country conduct many studies with patients and healthy volunteers. We have new and better treatment options today because of what clinical trials uncovered years ago. Be part of tomorrow’s medical breakthroughs. Talk to your health care provider about clinical trials, their benefits and risks, and whether one is right for you.
Reference
https://www.mayoclinic.org/diseases-conditions/bipolar-disorder/symptoms-causes/syc-20355955








It’s amazing to go to see this website and reading the views of all mates about
this piece of writing, while I am also eager of getting experience.
Excellent beat ! I would like to apprentice while you amend your site, how
could i subscribe for a weblog site? The account helped me a appropriate deal.
I had been a little bit acquainted of this your broadcast offered shiny clear idea
Just want to say your article is as surprising. The clearness in your post is simply excellent and i can assume you are an expert on this
subject. Well with your permission allow me to grab your RSS feed
to keep up to date with forthcoming post.
Thanks a million and please continue the enjoyable work.