Postpartum depression
Your body and mind go through many changes during and after pregnancy. If you feel empty, emotionless, or sad all or most of the time for longer than 2 weeks during or after pregnancy, reach out for help. If you feel like you don’t love or care for your baby, you might have postpartum depression. Treatment for depression, such as therapy or medicine, works and will help you and your baby be as healthy as possible in the future.
In this blog, Pritish Kumar gives some knowledgeable points about postpartum depression.
Postpartum depression is linked to chemical, social, and psychological changes that happen when having a baby. The term describes a range of physical and emotional changes that many new mothers experience. PPD can be treated with medication and counseling.
The chemical changes involve a rapid drop in hormones after delivery. The actual link between this drop and depression is still not clear. But what is known is that the levels of estrogen and progesterone, the female reproductive hormones, increase tenfold during pregnancy. Then, they drop sharply after delivery. By 3 days after a woman gives birth, the levels of these hormones drop back to what they were before pregnancy.
Who is affected by postpartum depression?
Postpartum depression is common. As many as 75% of people experience baby blues after delivery. Up to 15% of these people will develop postpartum depression. One in 1,000 people develop postpartum psychosis.

Signs and Symptoms
Symptoms of postpartum depression can be hard to detect. Many women have these symptoms following childbirth:
- Trouble sleeping
- Appetite changes
- Severe fatigue
- Lower libido
- Frequent mood changes
With PPD, these come along with other symptoms of major depression, which aren’t typical after childbirth, and may include:
- Being uninterested in your baby or feeling like you’re not bonding with them
- Crying all the time, often for no reason
- Depressed mood
- Severe anger and crankiness
- Loss of pleasure
- Feelings of worthlessness, hopelessness, and helplessness
- Thoughts of death or suicide
- notion of hurting someone else
- Trouble concentrating or making decisions

Symptoms of obsessive-compulsive disorder (OCD) that are new rarely occur in the postpartum period (about 1%-3% of women). The obsessions are usually related to concerns about the baby’s health or irrational fears of harming the baby. Panic disorder may also happen. You can have these conditions and depression at the same time.
Untreated postpartum depression can be dangerous for new moms and their children. A new mom should seek professional help when:
Symptoms persist beyond 2 weeks
- can’t function normally
- incapable to cope with everyday situations
- have thoughts of harming themselves or their baby
- feeling extremely anxious, scared, and panicked most of the day
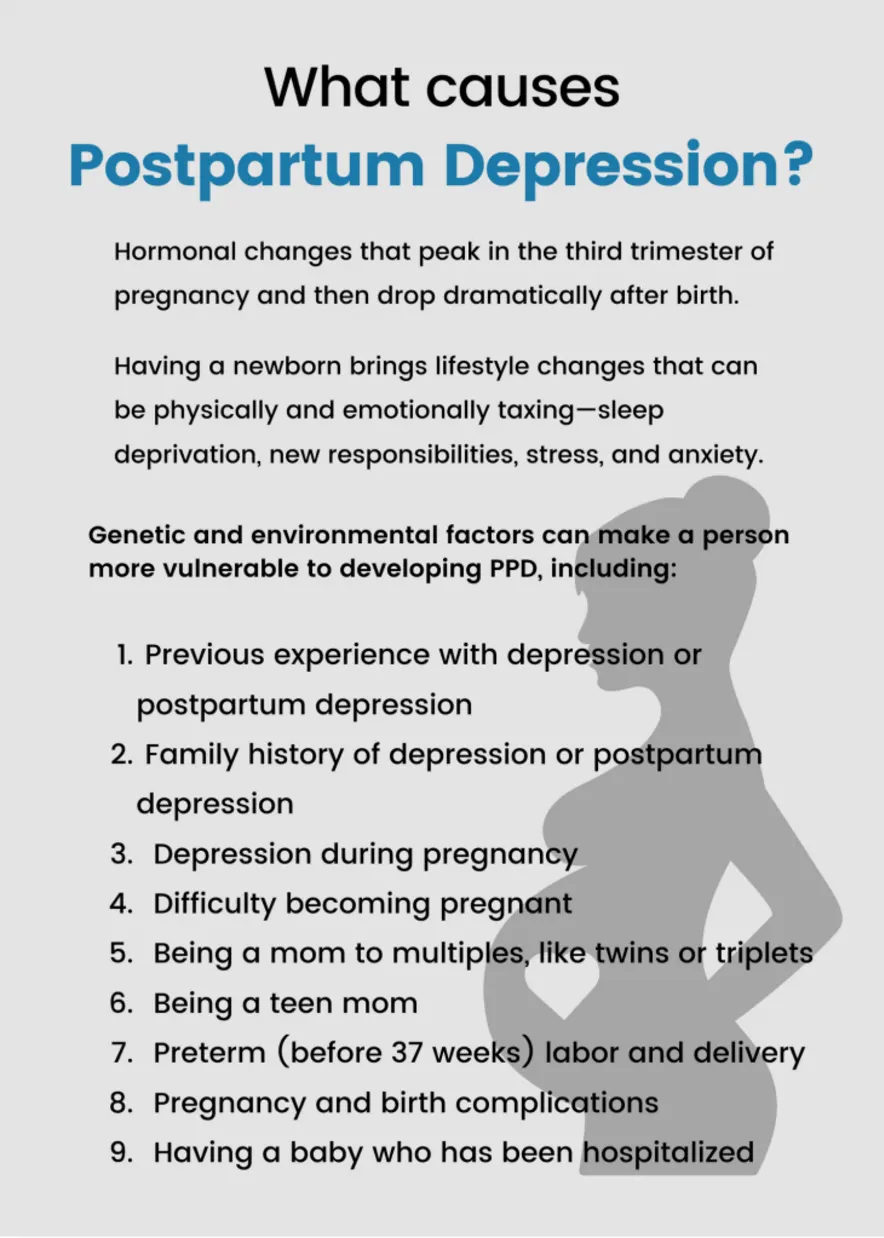
Causes and Risk Factors
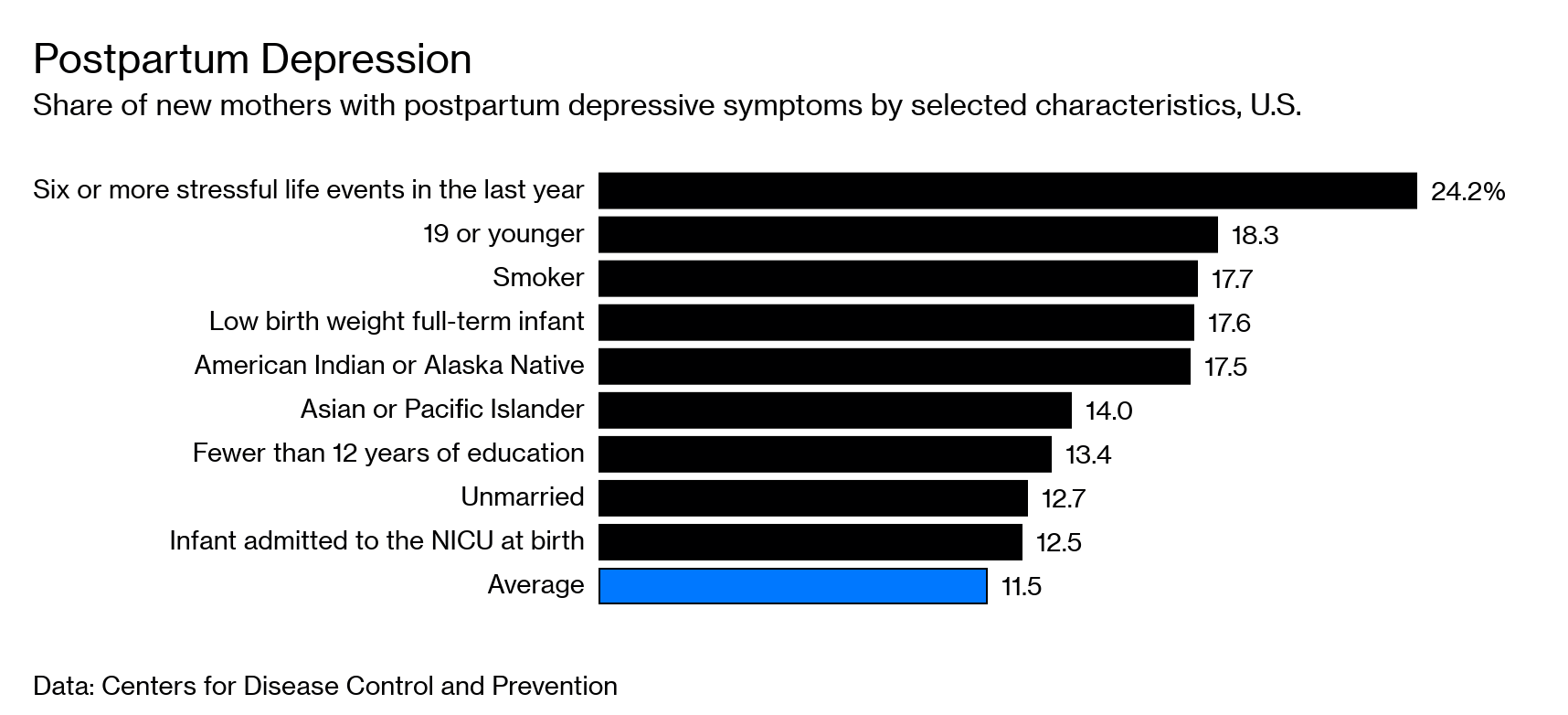
If you have PPD, it’s not because you did anything wrong. Experts think it happens for many reasons, and those can be different for different people. Some things that can raise the chances of postpartum depression include:
- A history of depression before becoming pregnant, or during pregnancy
- Age at time of pregnancy (the younger you are, the higher the chances)
- Ambivalence about the pregnancy
- Children (the more you have, the more likely you are to be depressed in later pregnancy)
- Family history of mood disorders
- Going through an extremely stressful event, like a job loss or health crisis
- Having a child with special needs or health problems
- twins or triplets
- a history of depression or premenstrual dysphoric disorder (PMDD)
- Limited social support
- Living alone
- Marital conflict
There’s no one cause of postpartum depression, but these physical and emotional issues may contribute:
Hormones. The dramatic drop in estrogen and progesterone after you give birth may play a role. Other hormones produced by your thyroid gland also may drop sharply and make you feel tired, sluggish, and depressed.
Lack of sleep. When you’re sleep-deprived and overwhelmed, you may have trouble handling even minor problems.
Anxiety. You may be anxious about your ability to care for a newborn.
Self-image. You may feel less attractive, struggle with your sense of identity, or feel that you’ve lost control over your life. Any of these issues can contribute to postpartum depression.
Types
There are three terms used to describe the mood changes women can have after giving birth:
The “baby blues” happen to as many as 70% of women in the days right after childbirth. You may have sudden mood swings, such as feeling very happy and then feeling very sad. You may cry for no reason and can feel impatient, cranky, restless, anxious, lonely, and sad. The baby blues may last only a few hours or as long as 1 to 2 weeks after delivery. Usually, you don’t need treatment from a health care provider for baby blues. Often, joining a support group of new moms or talking with other moms helps.
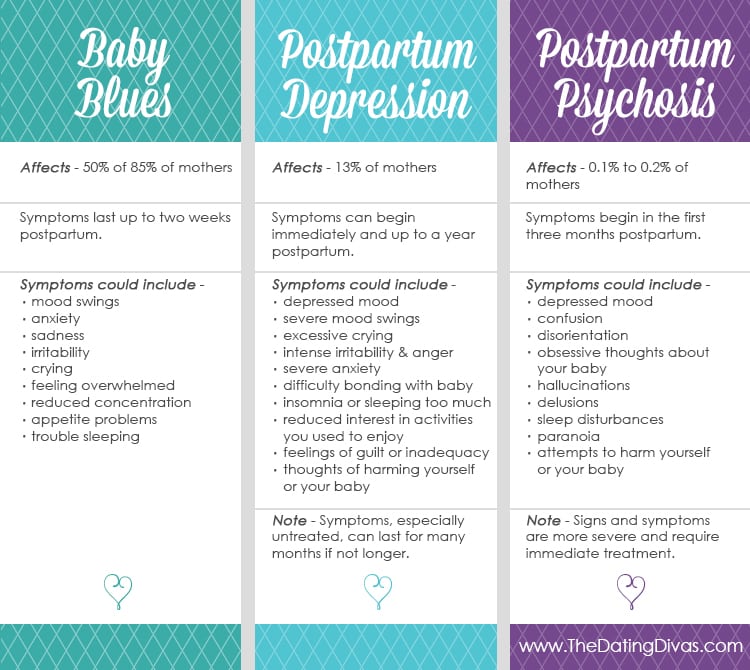
Postpartum depression (PPD) can happen a few days or even months after childbirth. PPD can happen after the birth of any child, not just the first child. You can have feelings similar to the baby blues — sadness, despair, anxiety, crankiness — but you feel them much more strongly. PPD often keeps you from doing the things you need to do every day. When your ability to function is affected, you need to see a health care provider, such as your OB/GYN or primary care doctor. This doctor can screen you for depression symptoms and come up with a treatment plan. If you don’t get treatment for PPD, symptoms can get worse. While PPD is a serious condition, it can be treated with medication and counseling.
Postpartum psychosis
This is a very serious mental illness that can affect new mothers. This illness can happen quickly, often within the first 3 months after childbirth. Women can lose touch with reality, have auditory hallucinations (hearing things that aren’t happening, like a person talking), and have delusions (strongly believing irrational things). Visual hallucinations (seeing things that aren’t there) are less common. Other symptoms include insomnia (not being able to sleep), feeling agitated and angry, pacing, restlessness, and strange feelings and behaviors. Women who have postpartum psychosis need treatment right away and almost always need medication. Sometimes women are put into the hospital because they are at risk of hurting themselves or someone else.
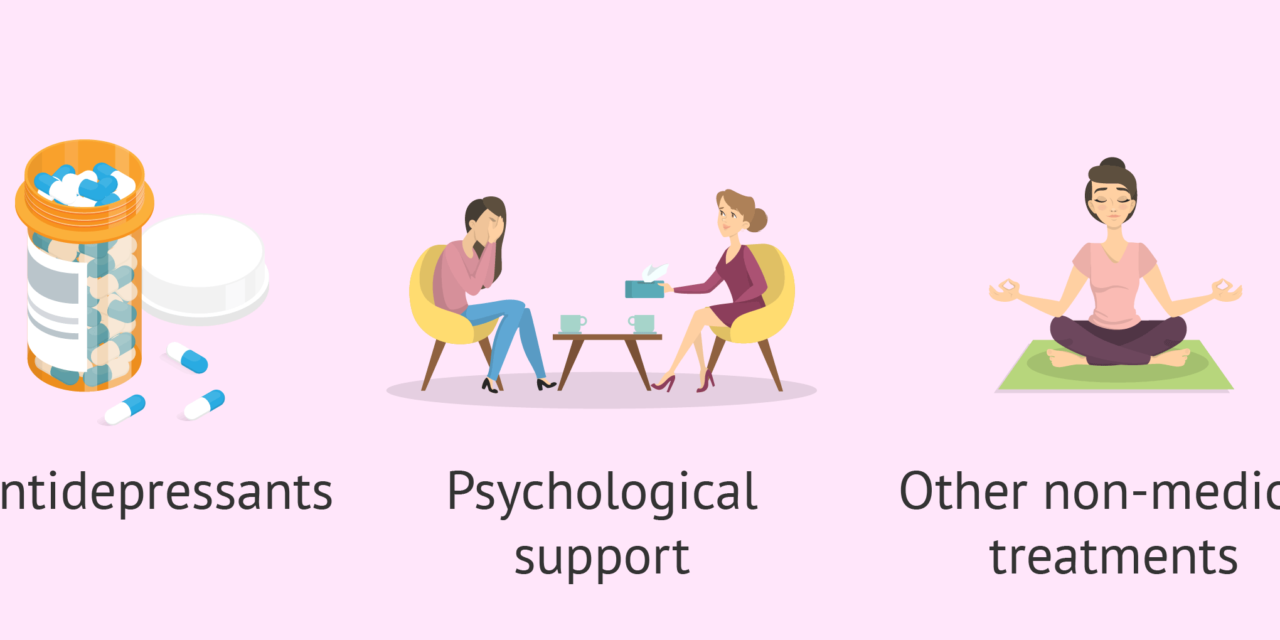
Treatment
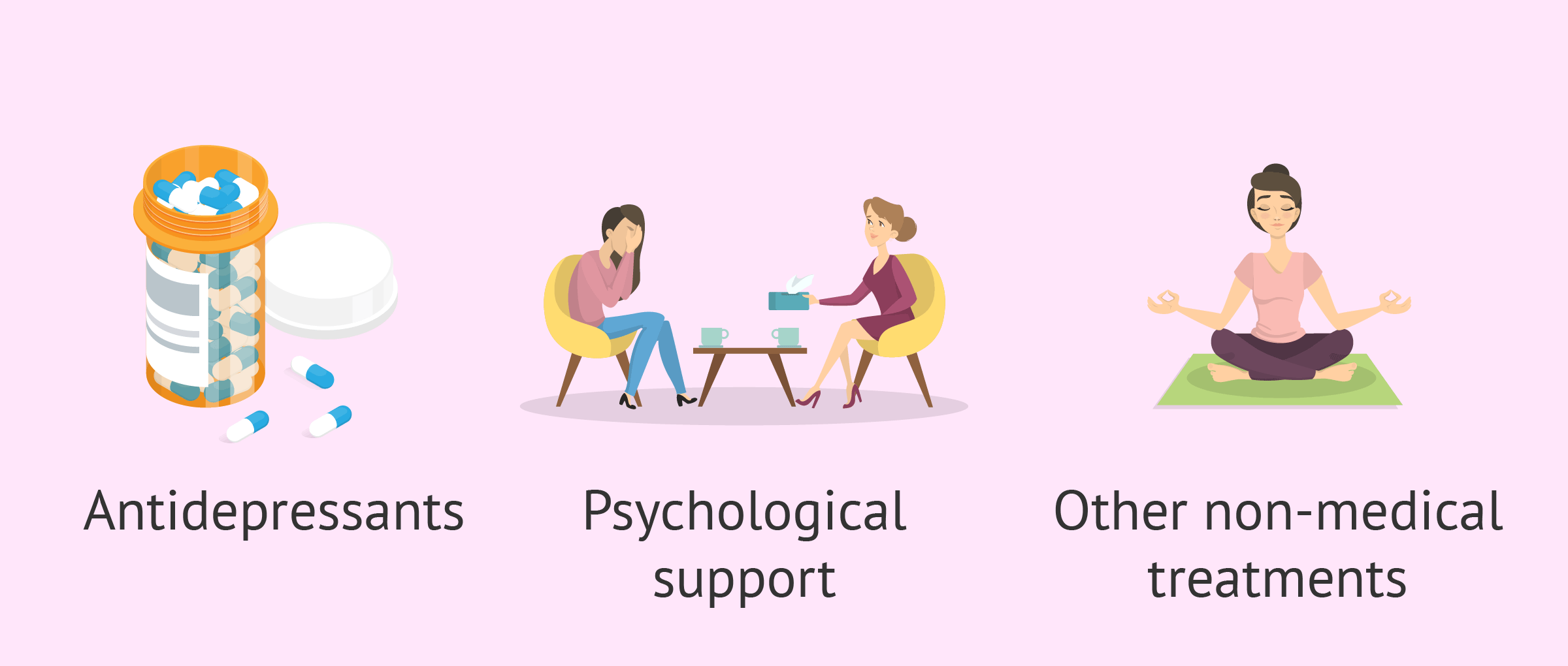
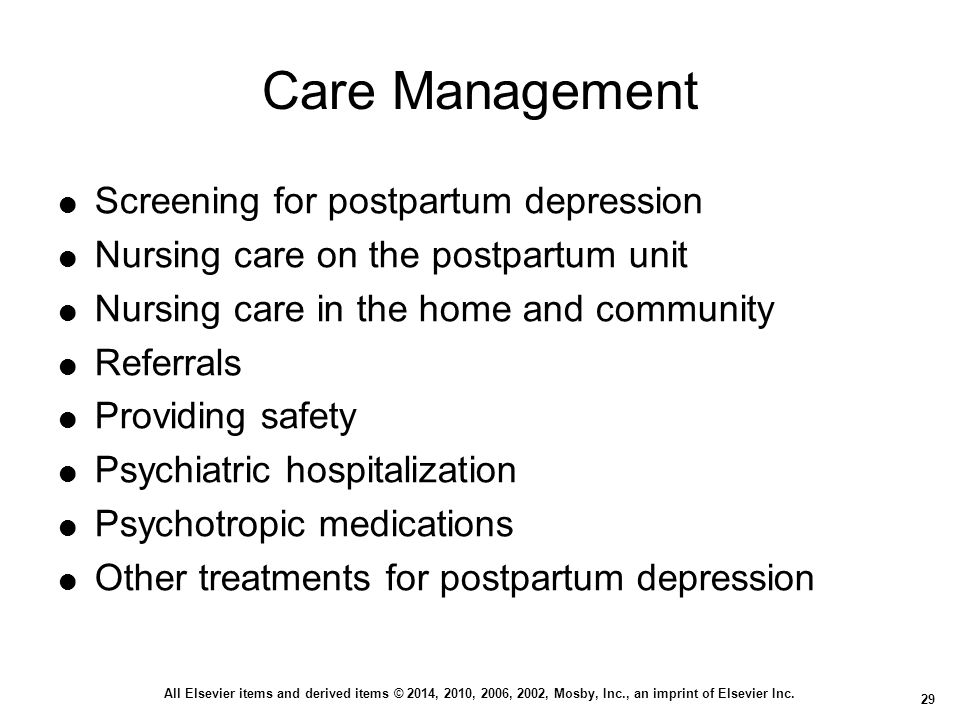
Postpartum depression is treated differently, depending on the type of symptoms and how severe they are. Treatment options include anti-anxiety or antidepressant medications, psychotherapy, and participation in a support group for emotional support and education. For severe cases, an IV of a new medication called brexanolone (Zulresso) may be prescribed.

In the case of postpartum psychosis, drugs used to treat psychosis are usually added. Hospital admission is also often necessary.
If you are breastfeeding, don’t assume that you can’t take medication for depression, anxiety, or even psychosis. Talk to your doctor. Under a doctor’s supervision, many women take medication while breastfeeding. This is a decision to be made between you and your doctor.
Complications
Postpartum depression that isn’t treated can weaken your ability to bond with your baby, and affect the whole family:
You. Postpartum depression that’s not treated can last for months or longer, even turning into a chronic depressive disorder. Even with treatment, postpartum depression can make you more likely to have episodes of depression in the future.
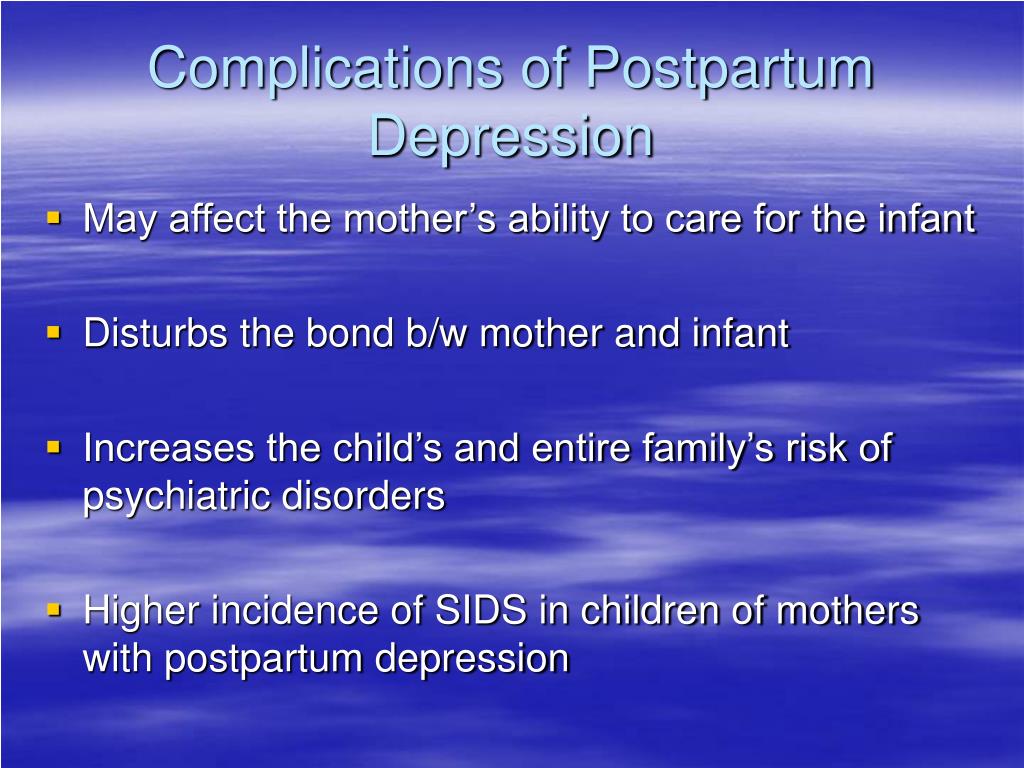
The baby’s father. When a new mother has depression, the father may be more likely to have depression too.
Children. Children of mothers with postpartum depression are more likely to have problems with sleeping and eating, crying more than usual, and delays in language development.
/Sad-dads-paternal-postpartum-depression-5120227-V1-e06edc0ce4f7481aafa129b2d027d34f.gif)
Postpartum Depression Prevention
If you have a history of depression, tell your doctor as soon as you find out you’re pregnant, or if you’re planning to become pregnant.
During pregnancy. Your doctor can monitor you for symptoms. You can manage mild depression symptoms with support groups, counseling, or other therapies. Your doctor may prescribe medications, even while you’re pregnant.
After your baby is born. Your doctor may recommend an early postpartum checkup to look for symptoms of depression. The earlier you’re diagnosed, the earlier you can begin treatment. If you have a history of postpartum depression, your doctor may recommend treatment as soon as you have the baby.

Managing after childbirth
Here are some tips that can help you cope with bringing home a newborn:

- Ask for help. Let others know how they can help you.
- Be realistic about your expectations for yourself and your baby.
- Exercise, within the limits of any restrictions your doctor may place on your level of activity; take a walk, and get out of the house for a break.
- Expect some good days and some bad days.
- Follow a sensible diet; avoid alcohol and caffeine.
- Foster the relationship with your partner — make time for each other.
- Keep in touch with family and friends — don’t isolate yourself.
- Limit visitors when you first go home.
- Screen phone calls.
- Sleep or rest when your baby sleeps.
How long does postpartum depression last?
Postpartum depression can last until one year after your child is born. However, this doesn’t mean you should feel “cured” in one year. Talk to your healthcare provider about your symptoms and treatment. Be honest about how you feel. Think carefully about if you feel better than you did at the beginning of your diagnosis. Then, they can recommend ongoing treatment for your symptoms.

Can postpartum depression affect my baby?
Yes, postpartum depression can affect your baby. Getting treatment is important for both you and your baby.
Research suggests that postpartum depression can affect your baby in the following ways:
- You have trouble bonding with your baby and don’t establish a connection with them.
- Your child may have behavior or learning problems.
- You may skip appointments with your child’s pediatrician.
- Your child may have feeding and sleeping issues.
- Your child may be at higher risk for obesity or developmental disorders.
- You may neglect your child’s care or not recognize when they are ill.
- Your baby may have impaired social skills.
Diagnosis
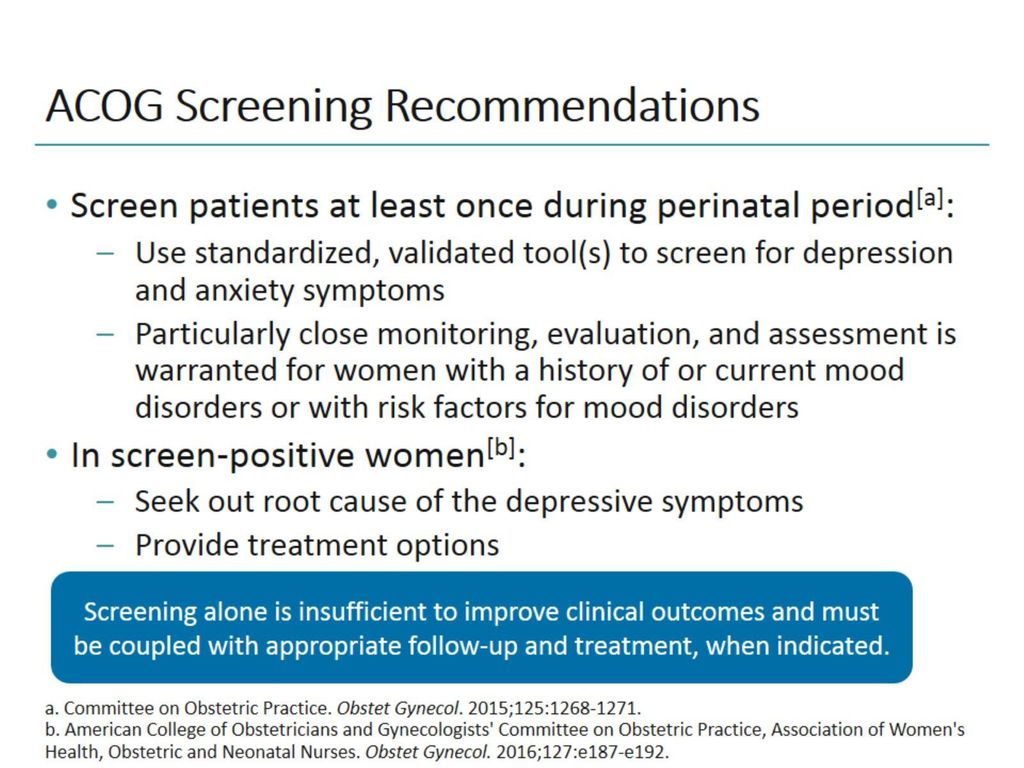
There is no specific test that diagnoses postpartum depression. Your healthcare provider will evaluate you at your postpartum visit. This visit may include discussing your health history, how you’ve felt since delivery, a physical exam, pelvic exam, and lab tests. Many providers schedule visits at two or three weeks postpartum to screen for depression. This ensures you get the help you need as soon as possible.
They may do a depression screening or ask you a series of
questions to assess if you have postpartum depression. They’ll ask how you’re feeling and how your baby is doing. Be open and honest with your provider to ensure they get an accurate picture of your emotions and thoughts. They can help distinguish if your feelings are typical or symptoms of postpartum depression.
Your healthcare provider may order a blood test because postpartum depression can cause symptoms similar to many thyroid conditions.
Remember, your healthcare provider is there to support you and make sure you are healthy, so be honest with them. There is no judgment, and you aren’t alone in your feelings.
Screening
It can be hard to detect mild cases of postpartum depression. Healthcare providers rely heavily on your responses to their questions.

Many healthcare providers use the Edinburgh Postnatal Depression Scale to screen for postpartum depression. It consists of 10 questions related to symptoms of depression such as feeling unhappy, anxious, or guilty. You’re asked to check the response that comes closest to how you’ve felt the last seven days. A higher score indicates possible postpartum depression.
If your provider feels you have signs of postpartum depression, they will recommend an appropriate treatment.
How is postpartum depression treated?
Postpartum depression is treated differently depending on the type and severity of your symptoms. Treatment options include anti-anxiety or antidepressant medicines, psychotherapy (talk therapy or cognitive behavioral therapy), and support group participation.
Treatment for postpartum psychosis may include medication to treat depression, anxiety, and psychosis. You may also be admitted to a treatment center for several days until you’re stable. If you don’t respond to this treatment, electroconvulsive therapy (ECT) can be effective.
If you are breastfeeding (chest feeding), don’t assume that you can’t take medicine for depression, anxiety, or even psychosis. Talk to your healthcare provider about your options.
Medications
Your healthcare provider may prescribe antidepressants to manage symptoms of postpartum depression. Antidepressants help balance the chemicals in your brain that affect your mood.
If you’re breastfeeding, talk to your healthcare provider about the risks and benefits of taking an antidepressant. Medications can transfer to your baby through your milk. However, the transfer level is generally low, and many antidepressant medications are considered safe. Your provider can help you decide what medicine is right for you based on your symptoms and if you’re nursing.
Some common antidepressants for postpartum depression are:
- Selective serotonin reuptake inhibitors (SSRIs) such as sertraline (Zoloft®) and fluoxetine (Prozac®).
- Serotonin and norepinephrine reuptake inhibitors (SNRIs) such as duloxetine (Cymbalta®) and desvenlafaxine (Pristiq®).
- Bupropion (Wellbutrin® or Zyban®).
Tricyclic antidepressants (TCAs) such as amitriptyline (Elavil®) or imipramine (Tofranil®).

Keep in mind that it takes at least three or four weeks for antidepressants to work. Talk to your healthcare provider before stopping the medication. Stopping your medication too soon can cause symptoms to return. Most providers will recommend reducing your dose before stopping completely.
If your provider detects postpartum depression while you’re still in the hospital, they may recommend IV medication containing brexanolone.
What are ways to cope with postpartum depression?
It’s OK to feel overwhelmed. Parenting is full of ups and downs and having a baby isn’t easy. If you have depression, you don’t have to suffer alone. Your healthcare provider can help find a treatment that works for you.
Here are some things you can do to help cope with postpartum depression:
Find someone to talk to — a therapist, friend, family member, or someone who will listen to you and help you.
- Join a support group for new parents.
- Try to eat healthily and find time for exercise.
- Prioritize rest for yourself.
- Go out with friends or talk to them on the phone.
- Find time for self-care and doing things you enjoy, like reading or other hobbies.
- Get help with household chores or errands.
What happens if postpartum depression isn’t treated?
Untreated postpartum depression is dangerous and affects you, your baby, and those who love you. It can make you:
- Feel like you have no energy.
- Believe you can’t take care of your baby.
- Unable to focus or make decisions.
- Have thoughts of hurting yourself.
PREVENTION
Can postpartum depression be prevented?

Postpartum depression isn’t entirely preventable. It helps to know the warning signs of the condition and what factors increase your risk. Here are some tips that can help prevent postpartum depression:
- Be realistic about your expectations for yourself and your baby.
- Limit visitors when you first go home.
- Ask for help — let others know how they can help you.
- Sleep or rest when your baby sleeps.
- Exercise — take a walk and get out of the house for a break.
- Keep in touch with your family and friends — don’t isolate yourself.
- Foster your relationship with your partner — make time for each other.
- Expect some good days and some bad days.
OUTLOOK / PROGNOSIS
What is the outlook for women with postpartum depression?
With professional help, almost all people who experience postpartum depression can overcome their symptoms.
Reference
https://www.womenshealth.gov/mental-health/mental-health-conditions/postpartum-depression
https://my.clevelandclinic.org/health/diseases/9312-postpartum-depression
https://www.webmd.com/depression/guide/postpartum-depression










I agree with your point of view, your article has given me a lot of help and benefited me a lot. Thanks. Hope you continue to write such excellent articles.