Overview
Depression is a mood disorder that causes a persistent feeling of sadness and loss of interest. Also called a major depressive disorder or clinical depression, it affects how you feel, think and behave and can lead to a variety of emotional and physical problems. You may have trouble doing normal day-to-day activities, and sometimes you may feel as if life isn’t worth living.

More than just a bout of the blues, depression isn’t a weakness and you can’t simply “snap out” of it. Depression may require long-term treatment. But don’t get discouraged. Most people with depression feel better with medication, psychotherapy, or both.
Depression Is Different From Sadness or Grief/Bereavement
The death of a loved one, loss of a job, or the ending of a relationship are difficult experiences for a person to endure. It is normal for feelings of sadness or grief to develop in response to such situations. Those experiencing loss often might describe themselves as being “depressed.”
But being sad is not the same as having depression. The grieving process is natural and unique to each individual and shares some of the same features of depression. Both grief and depression may involve intense sadness and withdrawal from usual activities. They are also different in important ways:
In grief, painful feelings come in waves, often intermixed with positive memories of the deceased. In major depression, mood and/or interest (pleasure) are decreased for most of the two weeks.
During sadness, self-esteem is usually maintained. In major depression, feelings of worthlessness and self-loathing are common.
Being in depression, thoughts of death may surface when thinking of or fantasizing about “joining” the deceased loved one. In major depression, thoughts are focused on ending one’s life due to feeling worthless or undeserving of living or being unable to cope with the pain of depression.
Grief and depression can co-exist For some people, the death of a loved one, losing a job, or being a victim of a physical assault, or a major disaster can lead to depression. When grief and depression co-occur, the grief is more severe and lasts longer than grief without depression.
Distinguishing between grief and depression is important and can assist people in getting the help, support, or treatment they need.
Risk Factors for Depression
Depression can affect anyone—even a person who appears to live in relatively ideal circumstances.
Several factors can play a role in depression:
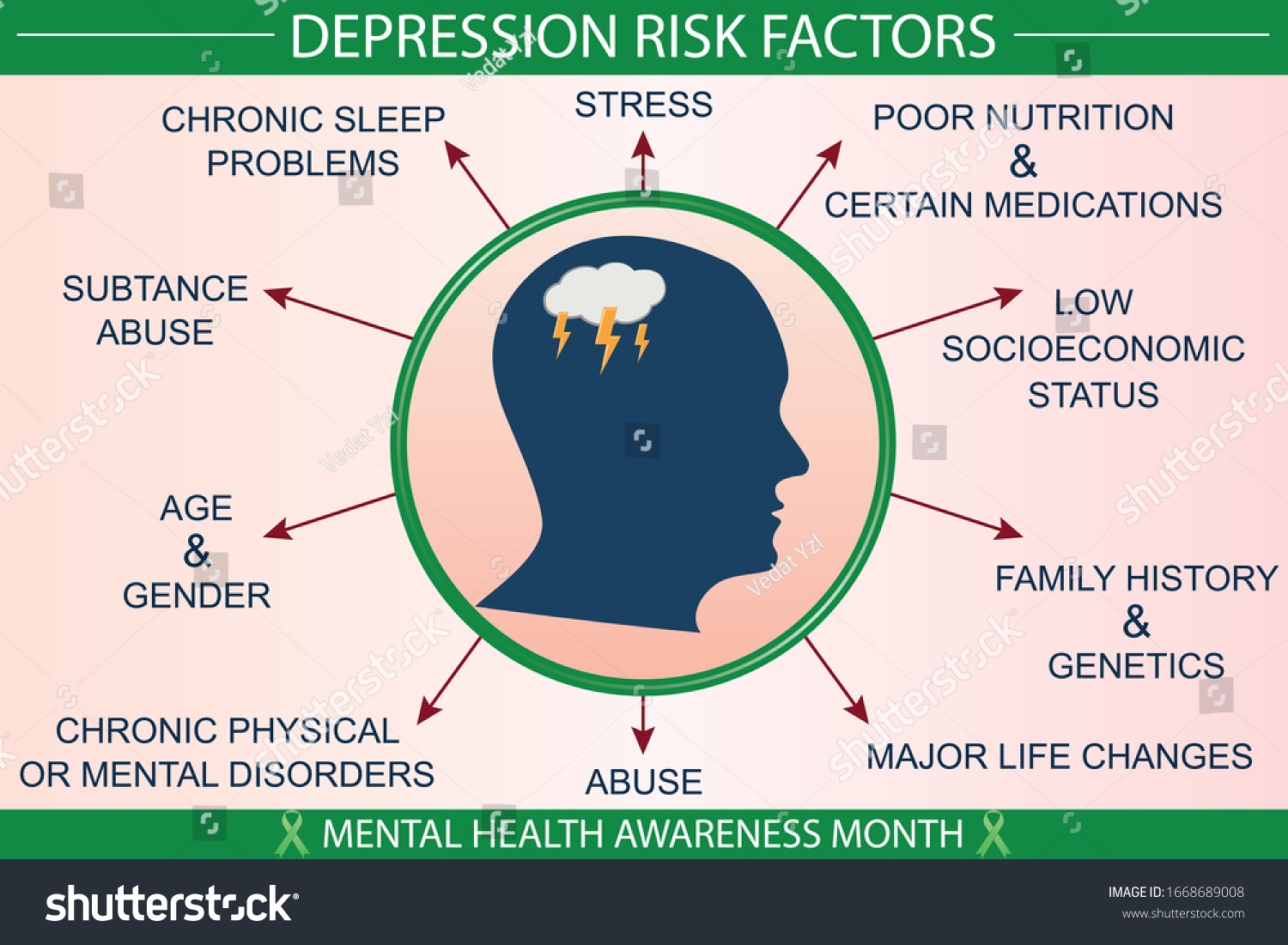
Biochemistry: Differences in certain chemicals in the brain may contribute to symptoms of depression.
Genetics: Depression can run in families. For example, if one identical twin has depression, the other has a 70 percent chance of having the illness sometime in life.
Personality: People with low self-esteem, who are easily overwhelmed by stress, or who are generally pessimistic appear to be more likely to experience depression.
Environmental factors: Continuous exposure to violence, neglect, abuse or poverty may make some people more vulnerable to depression.
Symptoms
Although depression may occur only once during your life, people typically have multiple episodes. During these episodes, symptoms occur most of the day, nearly every day, and may include:
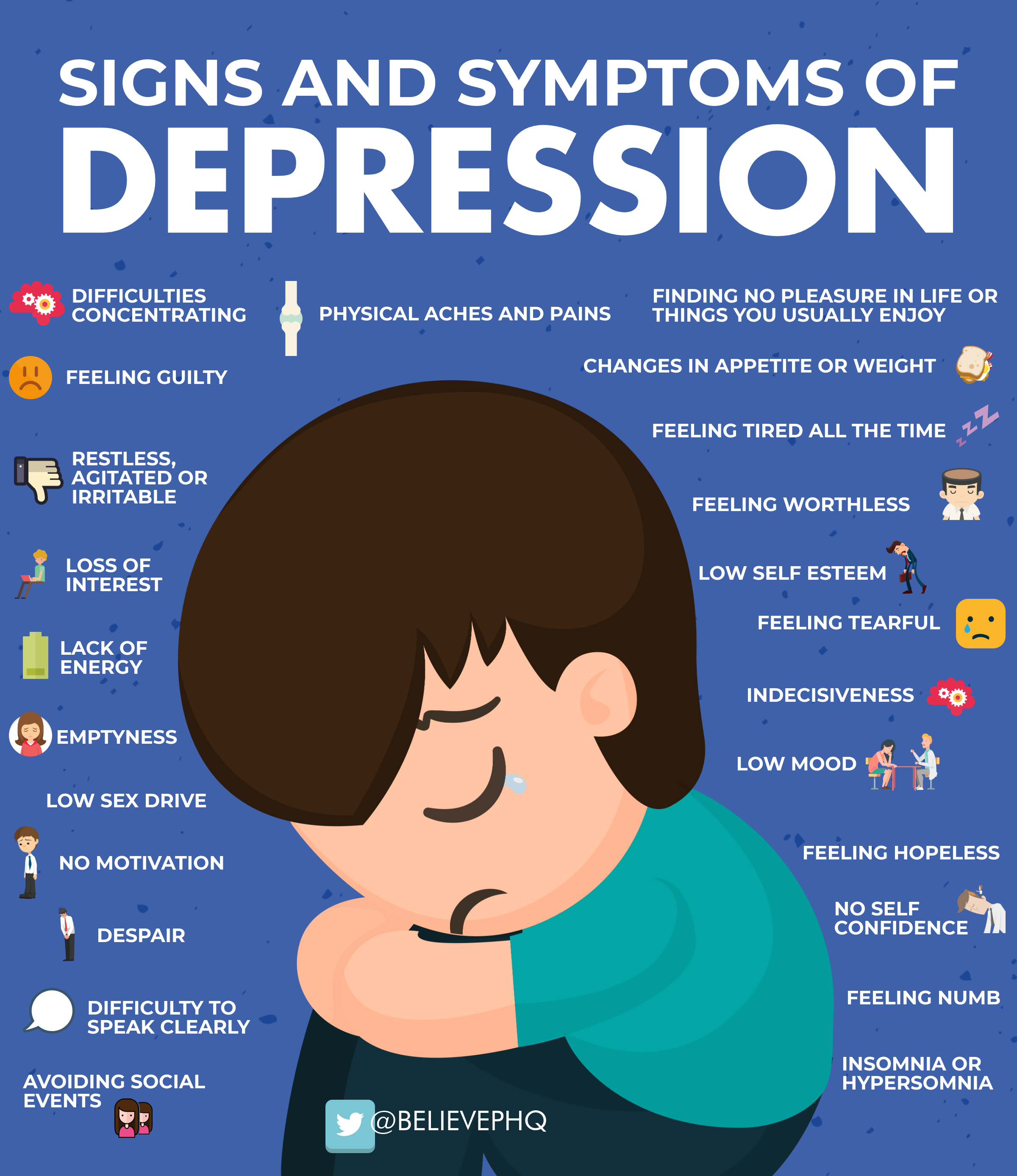
- Feelings of sadness, tearfulness, emptiness, or hopelessness
- Angry outbursts, irritability or frustration, even over small matters
- Loss of interest or pleasure in most or all normal activities, such as sex, hobbies, or sports
- Sleep disturbances, including insomnia or sleeping too much
- Tiredness and lack of energy, so even small tasks take extra effort
- Reduced appetite and weight loss or increased cravings for food and weight gain
- Anxiety, agitation, or restlessness
- Slowed thinking, speaking, or body movements
- Feelings of worthlessness or guilt, fixating on past failures or self-blame
- Trouble thinking, concentrating, making decisions, and remembering things
- Frequent or recurrent thoughts of death, suicidal thoughts, suicide attempts, or suicide
- Unexplained physical problems, such as back pain or headaches
For many people with depression, symptoms usually are severe enough to cause noticeable problems in day-to-day activities, such as work, school, social activities, or relationships with others. Some people may feel generally miserable without really knowing why.
Depression symptoms in children and teens
Common signs and symptoms of depression in children and teenagers are similar to those of adults, but there can be some differences.
In younger children, symptoms of depression may include sadness, irritability, clinginess, worry, aches, pains, refusing to go to school, or being underweight.

In teens, symptoms may include sadness, irritability, feeling negative and worthless, anger, poor performance or poor attendance at school, feeling misunderstood and extremely sensitive, using recreational drugs or alcohol, eating or sleeping too much, self-harm, loss of interest in normal activities, and avoidance of social interaction.
Depression symptoms in older adults
Depression is not a normal part of growing older, and it should never be taken lightly. Unfortunately, depression often goes undiagnosed and untreated in older adults, and they may feel reluctant to seek help. Symptoms of depression may be different or less obvious in older adults, such as:

- Memory difficulties or personality changes
- Physical aches or pain
- Fatigue, loss of appetite, sleep problems, or loss of interest in sex — not caused by a medical condition or medication
- Often wanting to stay at home, rather than going out to socialize or doing new things
- Suicidal thinking or feelings, especially in older men
When to see a doctor
If you feel depressed, make an appointment to see your doctor or mental health professional as soon as you can. If you’re reluctant to seek treatment, talk to a friend or loved one, any health care professional, a faith leader, or someone else you trust.
:max_bytes(150000):strip_icc()/illo_Doctor-discussion-guide-mind-08-5c60ad2a46e0fb000158767e.png)
When to get emergency help
If you think you may hurt yourself or attempt suicide, call 911 or your local emergency number immediately.
Also, consider these options if you’re having suicidal thoughts:
Call your doctor or mental health professional.
Call a suicide hotline number — in the U.S., call the National Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255). Use that same number and press “1” to reach the Veterans Crisis Line.

Reach out to a close friend or loved one.
Contact a minister, spiritual leader, or someone else in your faith community.
If you have a loved one who is in danger of suicide or has made a suicide attempt, make sure someone stays with that person. Call 911 or your local emergency number immediately. Or, if you think you can do so safely, take the person to the nearest hospital emergency room.
Reference
https://www.mayoclinic.org/diseases-conditions/depression/symptoms-causes/syc-20356007
https://psychiatry.org/patients-families/depression/what-is-depression